More Information
Submitted: August 06, 2024 | Approved: August 19, 2024 | Published: August 20, 2024
How to cite this article: Maharjan B, Singh J, Mishra SC, Neupane S. An Instance of Green-tinted Urine Related to the use of Propofol. Int J Clin Anesth Res. 2024; 8(1): 001-004. Available from: https://dx.doi.org/10.29328/journal.ijcar.1001024
DOI: 10.29328/journal.ijcar.1001024
Copyright License: © 2024 Maharjan B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Green urine; Propofol; Organophosphorus poisoning; Atropine; Case report
An Instance of Green-tinted Urine Related to the use of Propofol
Bindhya Maharjan*, Jeevan Singh, Shibesh Chandra Mishra and Saubhagya Neupane
MD, Department of Anesthesia, Dhulikhel Hospital, Kathmandu University School of Medical Sciences, Dhulikhel, Nepal
*Address for Correspondence: Bindhya Maharjan, MD, Department of Anesthesia, Dhulikhel Hospital, Kathmandu University School of Medical Sciences, Dhulikhel, Nepal, Email: bindhya.m18@gmail.com
Urine typically has an amber-yellow color due to the amorphous pigment urochrome, a distinct scent, and an average pH of 6.0, which is somewhat acidic. Green urine can result from drug intake, dyes, infections, adverse drug reactions, and other causes. Less than 1% of propofol users experience green urine, a rare and benign side effect. The green tint in urine is caused by the phenolic metabolites of propofol. In this case, a 33-year-old man diagnosed with organophosphorus poisoning and aspiration pneumonia had been given a modest dose of propofol sedation for six hours and began to exhibit green urine. After five hours of halting the propofol infusion, the urine returned to its usual color. Healthcare practitioners should be aware of this unusual but safe side effect of propofol.
Normal freshly voided urine has a distinct smell, an average pH of 6.0 that is slightly acidic, and an amber-yellow appearance due to the amorphous pigment urochrome. Green urine can result from drug intake, dyes, infections, side effects of drugs, and other conditions [1,2]. One often utilized intravenous anesthetic drug that is well-known for its ability to both induce and maintain anesthesia during medical operations is propofol. According to certain case reports, propofol rarely causes discoloration in the hair but can induce a visible green or pink-cloudy staining in the urine [3,4] Green urine is a rare and benign side effect that occurs in less than 1% of patients receiving propofol [5] Sigdel S. (2015) reported a case of propofol-induced green urine following a single induction dose in Nepal [6]. When administered for extended intravenous infusion, propofol is known to induce green urine [7]. The length of the continuous infusion has ranged from 6 to 64 hours [8]. It was noted that the discoloration resolved quickly, usually within two to three hours after the infusion was stopped, and was not linked to any complications [9]. Propofol is primarily eliminated in the urine as the 1-glucuronide, 4-glucuronide, and 4-sulfate conjugates of 2,6-diisopropyl-1,4-quinol after being metabolized in the liver [9]. These phenolic metabolites are responsible for the green coloring of urine. The metabolites do not reflect or alter renal function [3]. An intubated patient receiving propofol infusion was found to have green urine in this case report. The patient was diagnosed with organophosphorus poisoning and had normal liver function tests. Case reports documenting green urine in patients with organophosphorus poisoning who received propofol offer a novel insight into the interplay between these conditions and the anesthetic agent.
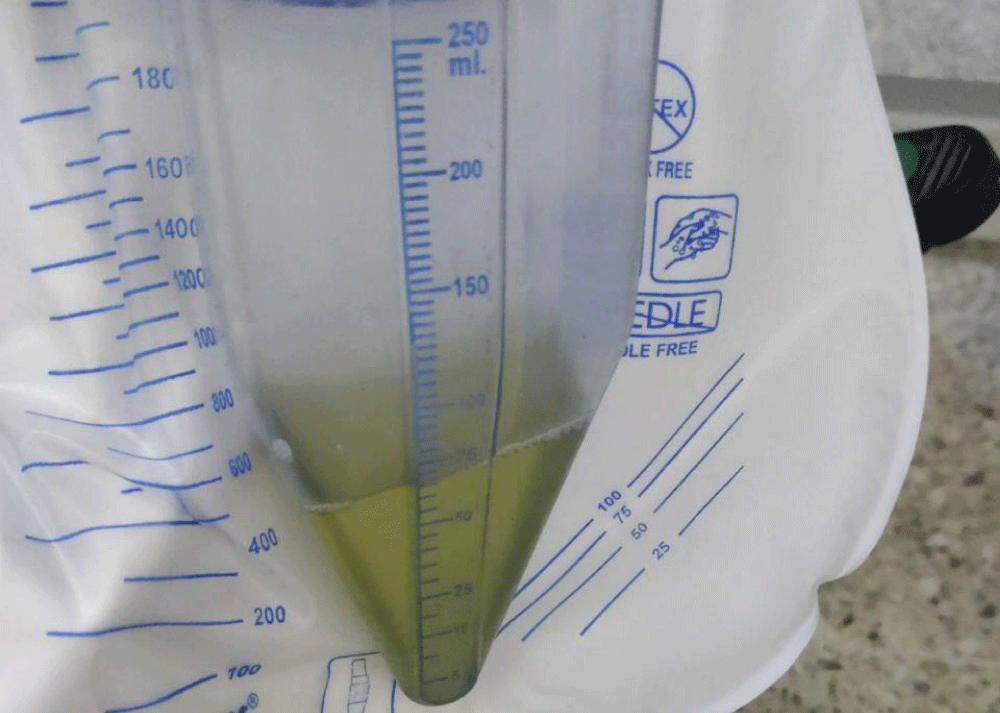
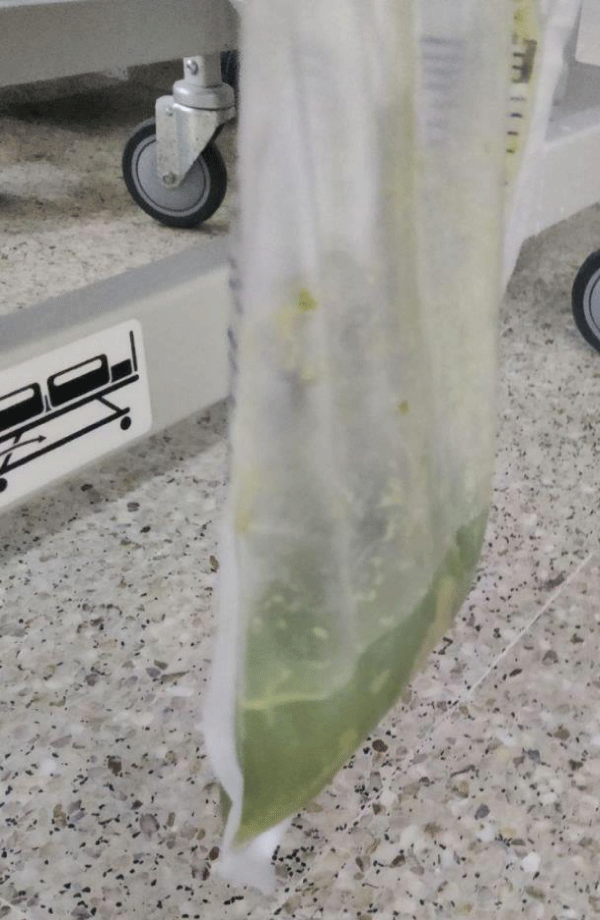
After being diagnosed with organophosphorus poisoning (using chlorpyrifos 50 and cypermethrin 5% EC pesticide), a 33-year-old male was admitted to the intensive care unit. Six hours before the patient’s presentation, he had ingested the insecticide while intoxicated. Poor oxygenation (SpO2–65% at 15 L O2 via facemask) and a GCS of 5/15 led to the patient’s intubation. The patient was placed on mechanical ventilation and admitted as a case of organophosphorus poisoning with aspiration pneumonia. The patient had a personal history of occasional smoking and consuming 400 milliliters of alcohol per day for the majority of the last ten years. There was no prior history of taking regular drugs and no notable surgical history. The patient received an injection of pralidoxime and regular titration of atropine infusion for organophosphorous poisoning. He was under mechanical ventilation for 11 days. During much of the intubation period, fentanyl and midazolam were used to maintain intravenous sedation. After 10 days of mechanical ventilation, propofol at a dose of 30 micrograms/kilogram/minute was used for sedation. After six hours of propofol sedation, green-colored urine was discovered in the uro bag, as depicted in Figure 1. Urine analysis results included green color, pus cells 1/High Power Field, and epithelial cells 3/High Power Field. His liver function test values were: serum bilirubin (direct) 0.2 mg/dL, total protein 6.2 gm/dL, aspartate aminotransferase 37 U/L, alanine aminotransferase 40 U/L, alkaline phosphatase 102 U/L, and total bilirubin 0.6 mg/dL. The picture in Figure 2 illustrates the green color of the nasogastric free drain bag collection, which was not previously the case. The renal function test was within normal limits. After 48 hours, there was no growth report from the urine culture sensitivity test. Following the event, the infusion of dexmedetomidine (0.3 mcg/kg/hr) was substituted for propofol. Normal yellowish-colored urine was collected in the uro bag 5 hours after the propofol infusion was stopped. On the fifth day of mechanical ventilation, the patient received a secondary diagnosis of ventilator-associated pneumonia, with a positive culture of Acinetobacter in the tracheal aspirate. The culture sensitivity report was followed when administering the injection of colistin. Better P/F ratios of more than 250 indicated that the oxygenation status was improving. The patient was not on any inotropes, and signs of sepsis were not present. The patient was extubated on the 12th day and shifted out of the ICU the next day.
Figure 1: Urometer filled with green coloured urine.
Figure 2: Nasogastric tube free drain bag partially mixed with leftover food particles and green coloured.
An intriguing and uncommon event sometimes observed in the context of anesthesia and critical care is green urine. Although Blakey, et al. estimated the phenomenon’s occurrence to be less than 1%, the precise incidence remains uncertain [9]. Substances consumed are the main cause of green urine in most situations. Green urine may result from medications such as amitriptyline, cetirizine, flutamide, indomethacin, methocarbamol, methylene blue, mitoxantrone, propofol, phenylbutazone, and triamterene. Potential dyes include carbolic acid, derivatives of flavone, indigo blue, indigo carmine, and methylene blue. It can also be caused by pathological conditions such as indicanemia, biliverdin, Pseudomonas infection, and Hartnup disease [7,10-12]. The presence of phenolic metabolites is responsible for the green tint of urine. Reports of green staining of hair following propofol medication also suggest these phenols [4,13].
Green urine is concerning, but it is not linked to propofol infusion syndrome, which is a dangerous condition characterized by sudden refractory bradycardia that can result in asystole, along with metabolic acidosis, rhabdomyolysis, hyperlipidemia, and an enlarged or fatty liver [14]. By obtaining a thorough history of the medications the patient has been prescribed or consumed, it is possible to identify the benign side effect of propofol that causes greenish discoloration of the urine. This can help prevent needless lab testing and the worry that comes with the unusual presentation. A quick urine test with a culture could aid in the diagnosis. Despite being fascinating, it is not very significant and doesn’t need to be treated unless it is an aftereffect of an infectious pathology.
An intriguing and uncommon event that is sometimes observed in the context of anesthesia and critical care is green urine. Although Blakey, et al. estimated the phenomenon’s occurrence to be less than 1%, the precise incidence remains uncertain [9]. Substances consumed are the main cause of green urine in most situations. Green urine may result from medications such as amitriptyline, cetirizine, flutamide, indomethacin, methocarbamol, methylene blue, mitoxantrone, propofol, phenylbutazone, and triamterene. Carbolic acid, derivatives of flavone, indigo blue, indigo carmine, and methylene blue are examples of potential dyes. It can also be caused by pathologic conditions such as indicanemia, biliverdin, Pseudomonas infection, and Hartnup disease [7,10-12]. The presence of these phenolic metabolites is responsible for the green tint of urine. Reports of green staining of hair following propofol medication also suggest these phenols [4,13].
The production of these phenolic compounds is enhanced by urine alkalinization and decreased by urine acidification [9]. Therefore green urine may be more commonly observed in patients who develop respiratory alkalosis while ventilated. In our instance, the pH levels were within the range of 7.30–7.45 based on multiple arterial blood gas analyses. Organophosphates are metabolized by the liver by oxidation and sulfate or glucuronate conjugation; oxidative damage may occur in the event of organophosphorus overdose. Hence, in cases of acute organophosphorus poisoning, liver enzymes such as SGOT and SGPT will be elevated [15]. While research on acute OP poisoning is scarce, studies on long-term OP exposure (in humans and animals) have shown a substantial increase in liver enzymes [16]. One of the most reliable and quick ways to gauge the extent of anticholinesterase pesticide poisoning is to measure the level of RBC cholinesterase in the blood. With a serum cholinesterase level of 328 U/l, less than 10% of normal, our patient was diagnosed with severe OP poisoning [17]. Nevertheless, our study’s results for Alanine aminotransferase, Aspartate aminotransferase, Direct Bilirubin, and Total Bilirubin did not indicate a significant correlation with the degree of poisoning. Atropine infusion was continued in this organophosphorus poisoning case at daily decreasing doses. Proximal gastric emptying is lessened by the cholinergic antagonist atropine [18]. Thus, we anticipate that decreased peristalsis resulting in impaired enterohepatic circulation may partially attenuate extra hepatic propofol glucuronidation. Furthermore, this may have eventually been connected to the development of green urine following a propofol infusion. Eri Takizawa, et al. concluded in their study that atropine administration increased the dose requirements for propofol induction of anesthesia and decreased propofol concentrations during constant infusion [14]. While this interaction may necessitate adjustments in dosing, it does not explicitly suggest an increase in side effects. To determine if atropine worsens propofol’s side effects, further investigation would be needed, focusing on adverse events and clinical outcomes associated with their combined use. Green urine is concerning, but it is not linked to propofol infusion syndrome, which is a dangerous condition characterized by sudden refractory bradycardia that can result in asystole when there is metabolic acidosis, rhabdomyolysis, hyperlipidemia, and an enlarged or fatty liver [19]. Green urine alone, without accompanying systemic symptoms, suggests a drug-related effect rather than propofol infusion syndrome. In contrast, propofol infusion syndrome presents with severe systemic manifestations [20]. Propofol infusion syndrome is more likely with prolonged high-dose infusions. If the green urine occurs with short-term or lower-dose propofol use, it’s less likely to be related to infusion syndrome. Green urine typically resolves with discontinuation or adjustment of propofol dosage, while symptoms of propofol infusion syndrome persist or worsen despite changes in treatment. By obtaining a thorough history of the medications the patient has been prescribed or consumed, it is possible to identify the benign side effect of propofol that causes greenish discoloration of the urine.
Our example illustrates a rare but harmless condition known as green urine staining, which is brought on by concurrent propofol dosing. Furthermore, in this case, a decrease in the amount of propofol glucuronidation in the intestine may have resulted from decreased enterohepatic circulation caused by atropine’s reduction of gastrointestinal motility. Propofol is widely utilized in anesthesia and intensive care unit sedation. Healthcare professionals need to be aware of this uncommon yet harmless side effect of propofol.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
- Shim YS, Gil HW, Yang JO, Lee EY, Kim SH, Hong SY. A case of green urine after ingestion of herbicides. Korean J Intern Med. 2008;23(1):42-44. Available from: https://doi.org/10.3904/kjim.2008.23.1.42
- Bowling P, Belliveau RR, Butler TJ. Intravenous medications and green urine. JAMA. 1981;246(3):216. Available from: https://pubmed.ncbi.nlm.nih.gov/7241760/
- Bodenham A, Culank LS, Park GR. Propofol infusion and green urine. Lancet. 1987;2(8561):740. Available from: https://doi.org/10.1016/s0140-6736(87)91097-x
- Callander CC, Thomas JS, Evans CJ. Propofol and the color green. Anesthesia. 1989;44(1):82. Available from: https://doi.org/10.1111/j.1365-2044.1989.tb11141.x
- Gonenavar MM, Shukla S, Sridhar T, Prasad R, Tabali R. An unusual instance of propofol-triggered green urine in anesthesia management: A case report. MGM J Med Sci. 2024;11:165-168. Available from: https://ouci.dntb.gov.ua/en/works/7njmXnm7/
- Sigdel S. Propofol induced green urine. J Anesth Clin Res. 2015;6(7):542. Available from: https://www.longdom.org/open-access-pdfs/propofol-induced-green-urine-2155-6148-1000542.pdf
- Ananthanarayan C, Fisher JA. Why was the urine green? Can J Anaesth. 1995;42(1):87-88. Available from: https://doi.org/10.1007/bf03010578
- Lee JS, Jang HS, Park BJ. Green discoloration of urine after propofol infusion. Korean J Anesthesiol. 2013;65(2):177-179. Available from: https://doi.org/10.4097/kjae.2013.65.2.177
- Blakey SA, Hixson-Wallace JA. Clinical significance of rare and benign side effects: propofol and green urine. Pharmacotherapy. 2000;20(9):1120-1122. Available from: https://doi.org/10.1592/phco.20.13.1120.35041
- Fulton B, Sorkin EM. Propofol. An overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs. 1995;50(4):636-657. Available from: https://doi.org/10.2165/00003495-199550040-00006
- Raymond JR, Yarger WE. Abnormal urine color: differential diagnosis. South Med J. 1988;81(7):837-841. Available from: https://doi.org/10.1097/00007611-198807000-00008
- Cooper C. What color is that urine specimen? Am J Nurs. 1993;93(8):37. Available from: https://doi.org/10.1097/00000446-199308000-00017
- Motsch J, Schmidt H, Bach A, Böttiger BW, Böhrer H. Long-term sedation with propofol and green discoloration of the liver. Eur J Anaesthesiol. 1994;11(6):499-502. Available from: https://pubmed.ncbi.nlm.nih.gov/7851359/
- Takizawa E, Takizawa D, Al-Jahdari WS, Miyazaki M, Nakamura K, Yamamoto K, et al. Influence of atropine on the dose requirements of propofol in humans. Drug Metab Pharmacokinet. 2006;21(5):384-388. Available from: https://doi.org/10.2133/dmpk.21.384
- Jelia SC, Lal B, Airan D. Biochemical indicators and the Peradeniya Organophosphate Poisoning scale in prediction and prognosis of organophosphorus poisoning: An observational prospective study. J Acute Dis. 2023;12(4):133-139. Available from: http://dx.doi.org/10.4103/2221-6189.385679
- Senarathne R, Hettiaratchi U, Athiththan L, Peiris H, Sarathchandra C, Senanayake H, Weerawansa P, Siribaddana S. Selected liver markers in predicting the severity of organophosphate and carbamate poisoning. J Environ Public Health. 2022;2022:7826396. Available from: https://doi.org/10.1155/2022/7826396
- Chaudhary SC, Singh K, Sawlani KK, Jain N, Vaish AK, Atam V, Patel ML, Agarwal A. Prognostic significance of estimation of pseudocholinesterase activity and role of pralidoxime therapy in organophosphorous poisoning. Toxicol Int. 2013;20(3):214-217. Available from: https://doi.org/10.4103/0971-6580.121669
- Parkman HP, Trate DM, Knight LC, Brown KL, Maurer AH, Fisher RS. Cholinergic effects on human gastric motility. Gut. 1999;45(3):346-354. Available from: https://doi.org/10.1136/gut.45.3.346
- Loh N, Nair P. Propofol infusion syndrome. Contin Educ Anaesth Crit Care Pain. 2013;13(6):200-202. Available from: http://dx.doi.org/10.1093/bjaceaccp/mkt007
- Singh A, Anjankar AP. Propofol-related infusion syndrome: A clinical review. Cureus. 2022;14(10):e30383. Available from: https://doi.org/10.7759/cureus.30383