More Information
Submitted: 22 September 2020| Approved: 09 November 2020 | Published: 10 November 2020
How to cite this article: Baygin M, Koltuk M, Koseoglu BG. Nasopalatin duct cysts: Report of ten cases and review of literature. Int J Clin Anesth Res. 2020; 4: 019-022.
DOI: 10.29328/journal.ijcar.1001016
Copyright License: © 2020 Baygin M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Nasopalatin duct cysts: Report of ten cases and review of literature
Melike Baygin*, Melek Koltuk and Banu Gurkan Koseoglu
Faculty of Dentistry, Oral and Maxillofacial Surgery, Istanbul University, Turkey
*Address for Correspondence: Melike Baygin, Faculty of Dentistry, Oral and Maxillofacial Surgery, Istanbul University, Turkey, Tel: +905543362625; Email: melikebaygin.mb@gmail.com
Nasopalatine duct cyst is the most common non-odontogenic cyst. It develops in the midline of the anterior maxilla. It is usually asymptomatic and sometimes it can be overlooked or misdiagnosed. We present 10 patients who applied to Istanbul University Faculty of Dentistry, Department of Oral and Maxillofacial Surgery.
Nasopalatine duct cyst, also known as incisive canal cyst, is the most common among non-odontogenic developmental cysts [1-3]. It occurs in approximately 1% of the population [4]. It was first described by Meyer in 1914 [4]. Nasopalatine duct cyst, which is more common in 4-6th decades, mostly develops in the midline of the anterior maxilla [5,6]. This cyst is more frequent in male [5]. Most patients are asymptomatic. When they are symptomatic, they present as swelling of anterior hard palate, sometimes associated with pain and drainage [7]. They must usually be larger than 0.6 cm to distinguish cyst from incisive foramen, which is a normal anatomical feature. They are seen as a solitary well-defined, oval or round unilocular radiolucency, between central incisors, >0.6 cm in diameter [7,8]. They may appear “heart-shaped” if the anterior nasal spine superimposed. Root resorption and tooth displacement may be present.Enucleation is usually curative, and recurrence is rare. Histological confirmation is recommended [7].
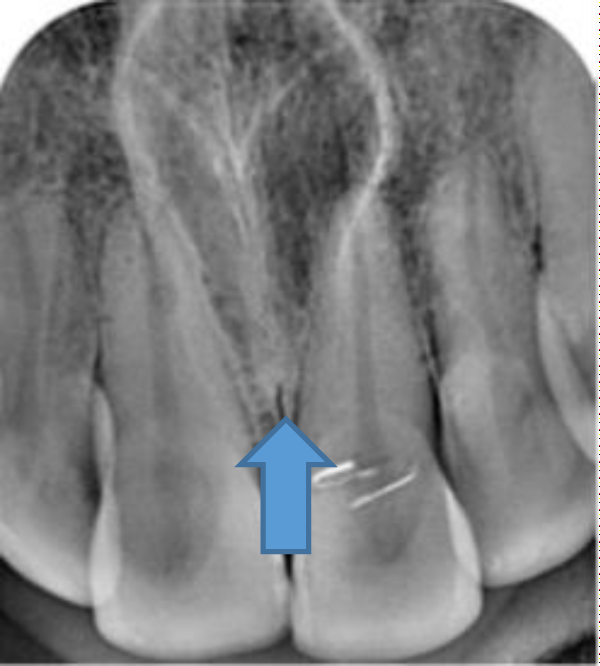
We present the case of nasopalatine canal cyst in 10 patients, 8 males and 2 females, aged between 34-66, who applied to Istanbul University Faculty of Dentistry, Department of Oral and Maxillofacial Surgery. We examined the patients in terms of age (years), gender, complaints, radiographic findings and the condition of the teeth involved. Nasopalatine duct cyst was detected on routine radiography in 2 patients, and 2 patients complained of saltwater taste in the mouth. Six patients complained of swelling they felt in the palatinal region (Figure 1). Panoramic radiography showed heart shaped radiolucent area in 3 patients and 7 patients had oval radiolucent area (Figures 2,3).
Figure 1: Intraoral view. Swelling in the palatine.
Figure 2: Nasopalatine duct cyst with a heart-shaped image.
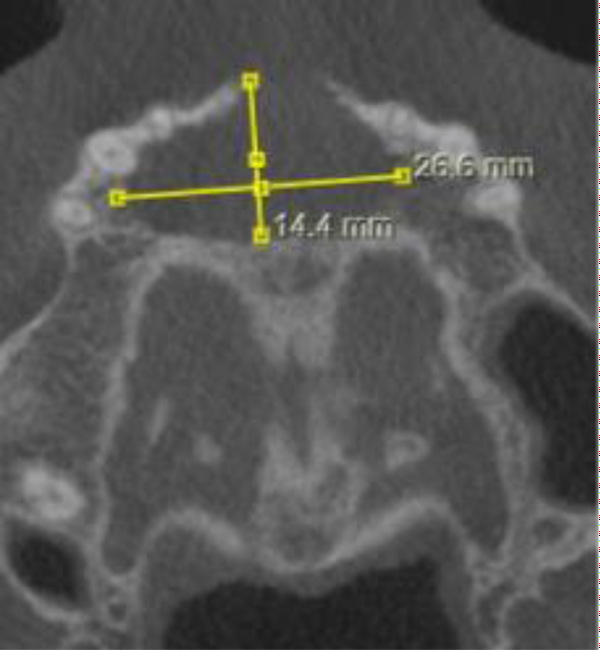
Figure 3: Horizontal CBCT view.
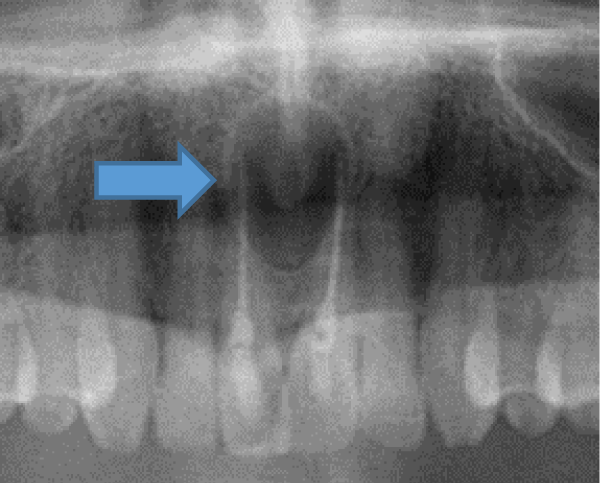
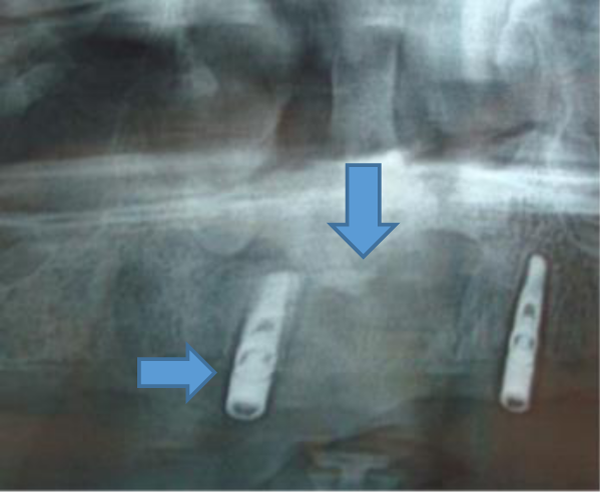
When the conditions of the related teeth were evaluated, it was observed that the teeth were devital in 3 patients, the implant was inside the lesion in 1 patient, 1 patient was toothless, and the related teeth were vital in 5 patients (Figures 4,5).
Figure 4: Nasopalatine canal cyst misdiagnosed as periapical granuloma and teeth with root canal treatment.
Figure 5: Nasopalatine duct cyst was not noticed and dental implant was placed. Heart-shaped radiolucent lesion.
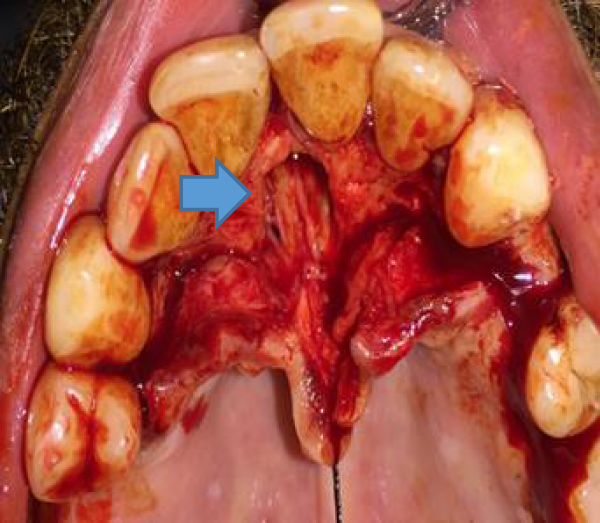
Nasopalatine duct cysts are usually treated by enucleation through the palatinal approach [5]. Surgical enucleation of the cyst is performed under local anesthesia and the result is generally positive when the cyst is aspirated before removal. We enucleated all cysts under local anesthesia (Figures 6,7).
It has a good prognosis. No recurrence was observed in the patients we followed up.
Figure 6: Intraoperative image.
Figure 7: Enucleated nasopalatine duct cyst.
| Table 1: Summary of cases of patients with nasopalatin duct cyst. | ||||
| Age (years) | Gender | Complaınt | Radıography | Condıtıon of the teeth |
| 47 | Male | Noticed on routine radiography | Oval radiolucent lesion | Vital |
| 51 | Male | Swelling in the palatinal area | Oval radiolucent lesion | Vital |
| 34 | Male | Noticed on routine radiography | Oval radiolucent lesion | Vital |
| 47 | Male | Salty taste | Oval radiolucent lesion | Devital |
| 65 | Male | Swelling in the palatinal area | Heart shaped radiolucent lesion | Vital |
| 65 | Male | Swelling in the palatinal area | Oval radiolucent lesion | Devital |
| 35 | Female | Swelling in the palatinal area | Oval radiolucent lesion | Vital |
| 66 | Male | Salty taste | Heart shaped radiolucent lesion | Implant |
| 48 | Male | Swelling in the palatinal area | Oval radiolucent lesion | Devital |
| 35 | Female | Swelling in the palatinal area, prosthesis doesn’t fit. | Heart shaped radiolucent lesion | Edentate |
Nasopalatine duct cysts, which can be seen at any age, are more common in 4-6th decades [2]. It is observed three times more frequently in males than in females [2]. In our cases, male patients are the majority and the average age of the patients is 49.4. These results are similar to the literature [5,7,8]. Panoramic radiography, periapical radiography, occlusal radiography and computed tomography can be used in radiological examination [2]. Especially periapical radiographs taken from different horizontal angles facilitate the diagnosis. In this control, the appearance of the nasopalatine canal cyst changes, while the radicular cyst continues to be located at the apex of the central incisors [2,6]. Incisive foramen larger than 6 mm may give the appearance of cysts [8]. Follow-up radiographs should be taken in suspected cases [6]. Nasopalatine duct cyst is well circumscribed, giving a round or oval appearance [6]. The shadow of the nasal spina sometimes can be superposed, causing the cyst to look like a heart shaped [2]. We found mostly oval shaped radiolucent lesions in the cases we presented. Radiographic images of 3 patients have a heart-shaped radiolucent area.
The radiographic image is not always symmetric, it can give the same image as the radicular cyst and periapical granuloma [2,6]. Aparna, et al. presented a case of nasopalatine duct cyst that was mistaken for radicular cyst and was treated incorrectly. They reported that there were 8 similar cases in the literature [9]. Loss or enlargement of the lamina dural at the apex of the central incisors indicates an inflammatory lesion [2,9]. Vitality test is very important in differential diagnosis. In the nasopalatine duct cyst, the teeth maintain their vitality [3,6,9]. 3 patients whose complaints did not resolve even though their teeth had root canal treatment, applied to our clinic. Nasopalatine duct cysts diagnosed after enucleation. Clinical and radiographic improvement was observed after the enucleation of the cysts. This situation confirms that the related teeth are vital in the nasopalatine duct cyst and can be misdiagnosed radiographically with other periapical pathologies.
Nasopalatine canal cyst is mostly asymptomatic and diagnosed on routine radiography. The most common symptoms are swelling, pain, and drainage of the anterior palate mucosa. Near-surface cysts can cause blue, fluctuant swelling in this area. Deep cysts are covered with normal mucosa as long as there is no ulceration. If nasopalatine nerve is pressed, burning and numbness may occur in the area [2].
When it drains into the mouth, patient can feel salty taste. A 66-year-old male patient applied to our clinic complained of the salt water taste he felt in his mouth. After the panoramic radiography, it was observed that the nasopalatine canal cyst was not noticed, and a dental implant was placed into it. There are 4 implant-related nasopalatine duct cyst cases in the literature [10]. In all cases, nasopalatine duct cyst developed after implant surgery [10]. Cyst development in 3 cases was attributed to the traumatization of the nasopalatine duct [11,12]. In one case, it was reported that cellular proliferation might have been induced by infection in the area [13]. In our case (Figure 5), the nasopalatine canal cyst was not noticed in the radiological examination and the dental implant was placed in the cyst.
Nasopalatine duct cyst is generally asymptomatic and can be detected on routine radiographs. Sometimes, it can cause swelling, drainage or pain in the palatal mucosa. Although panoramic radiography is accepted as the standard in the first approach to pathological formations in the jaws, the superposed image may mislead the physician. In case of doubt, besides panoramic radiography, auxiliary diagnostic methods such as computed tomography, periapical graphy, vitality test should be used. It must be distinguished from other maxillary anterior radiolucencies to prevent a wrong treatment plan. The final diagnosis is made as a result of histopathological examination. Enucleation is the preferred treatment method because of its low recurrence rate.
- Grossmann SM, Machado VC, Xavier GM, Moura MD, Gomez RS, Aguiar MC, et al: Demographic profile of odontogenic and selected nonodontogenic cysts in a Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104: e35-e41. PubMed: https://pubmed.ncbi.nlm.nih.gov/17942344/
- Shylaja S, Balaji K, Krishna A: Nasopalatine duct cyst: report of a case with review of literature. Indian J Otolaryngol Head Neck Surg. 2013; 65: 385-388, 2013. PubMed: https://pubmed.ncbi.nlm.nih.gov/24427606/
- Silva Barros C, Pontes Santos HB, Cavalcante I, Amaral Rolim LS, Pinto LP, de Souza LB. Clinical and histopathological features of nasopalatine duct cyst: A 47-year retrospective study and review of current concepts. J Cranio-Maxillo-Facial Sur. 2018; 46: 264-268. PubMed: https://pubmed.ncbi.nlm.nih.gov/29248496/
- Shylaja S, Balaji K, Krishna A. Nasopalatine Duct Cyst: Report of a Case with Review of Literature. Indian J Otolaryngol Head Neck Surg. 2013; 65: 385–388. PubMed: https://pubmed.ncbi.nlm.nih.gov/24427606/
- Francolí JE, Marqués NA, Aytés LB, et al. Nasopalatine duct cyst: report of 22 casesand review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13: E438–443. PubMed: https://pubmed.ncbi.nlm.nih.gov/18587308/
- Srivastava S.Misra N,Agarwal R,Pandey P. Nasopalatine canal cyst: often missed. BMJ Case Rep 2013. PubMed: https://pubmed.ncbi.nlm.nih.gov/23536642/
- Elliott KA, Franzese CB, Pitman KT: Diagnosis and surgical management of nasopalatine duct cysts. Laryngoscope. 2004; 114: 1336-1340. PubMed: https://pubmed.ncbi.nlm.nih.gov/15280704/
- Çakarer S, Tekkeşin Soluk M. ‘çene kemiklerinin kistleri’. Ed. Alpaslan C. Ağız, diş ve çene cerrahisi. Kanıta dayalı tanı ve tedavi yaklaşımları. Quntessence Publishing. 2018; 315-332.
- Aparna M,Chakravarthy A,Acharya SR,Radhakrishnan R. A clinical report demonstrating the significance of distinguishing a nasopalatine duct cyst from a radicular cyst. BMJ Case Rep. 2014; 2014: bcr2013200329. PubMed: https://pubmed.ncbi.nlm.nih.gov/24642171/
- Al-Shamiri HM, Elfaki S, Al-Maweri SA, Alaizari NA, Tarakji B. Development of Nasopalatine Duct Cyst in Relation to Dental Implant Placement. N Am J Med Sci. 2016; 8: 13-16. PubMed: https://pubmed.ncbi.nlm.nih.gov/27011942/
- McCrea SJ. Nasopalatine duct cyst, a delayed complication to successful dental implant placement: Diagnosis and surgical management. J Oral Implantol. 2014; 40: 189–195. PubMed: https://pubmed.ncbi.nlm.nih.gov/24779952/
- Sivolella S, Valente M, Gasparini E, Stellini E. Nasopalatine duct cyst as a complication of dental implant placement: A case report. Minerva Stomatol. 2013; 62: 235–239. PubMed: https://pubmed.ncbi.nlm.nih.gov/23828259/
- Casado PL, Donner M, Pascarelli B, Derocy C, Duarte ME, Barboza EP. Immediate dental implant failure associated with nasopalatine duct cyst. Implant Dent. 2008; 17: 169–175. PubMed: https://pubmed.ncbi.nlm.nih.gov/18545048/
- Gnanasekhar JD, Walvekar SV, Al-Kandari AM, Al-Duwairi Y. Misdiagnosis and mismanagement of a nasopalatine duct cyst and its corrective therapy. A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80: 465-470. PubMed: https://pubmed.ncbi.nlm.nih.gov/8521111/
- Neville BW, Damm DD, Allen CM, et al. Oral and maxillofacial pathology. In: Developmental defects of the oral and maxillofacial region. 2nd edn. Philadelphia,USA: Saunders, 2005:27–30.
- Regezi JA, Sciubba JJ, Jordan RCK. Oral pathology clinical pathologic correlations. In: Rudolph P, ed. Cysts of the jaws and neck. 4th edn. San Francisco, USA:Saunders. 2003: 256–257.
- Shear M, Speight PM. Nasopalatine duct cyst. In: Cysts of the oral and maxillofacial regions. 4th edn. Oxford, UK: Blackwell Munksgaard. 2007: 108–113.
- White SC, Pharoah MJ. Cysts of the jaws. In: Rudolph P, ed. Oral radiology principles and interpretation. 5th edn. St. Louis, USA: Mosby, 2004:400–401.
- Takeshita K, Funaki K, Jimbo R, Takahashi T. Nasopalatine duct cyst developed in association with dental implant treatment: A case report and histopathological observation. J Oral Maxillofac Pathol. 2013; 17: 319. PubMed: https://pubmed.ncbi.nlm.nih.gov/24250105/