More Information
Submitted: 05 June 2020| Approved: 11 June 2020 | Published: 15 June 2020
How to cite this article: Nasibova EM. The choice of optimal modern muscle relaxants (rocuronium bromide, atracurium besilate and cisatracurius besilate) in one-day surgery in children. Int J Clin Anesth Res. 2020; 4: 004-012.
DOI: 10.29328/journal.ijcar.1001014
Copyright License: © 2020 Nasibova EM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ideal muscle relaxant; Rocuronium bromide; Atracurium besilate; Cisatracurium besilate
The choice of optimal modern muscle relaxants (rocuronium bromide, atracurium besilate and cisatracurius besilate) in one-day surgery in children
Nasibova EM*
Azerbaijan Medical University, Baku, Azerbaijan
*Address for Correspondence: Nasibova EM, Azerbaijan Medical University, Baku, Azerbaijan, Tel: +994503366077; Email: doc.nasibova.esmira@gmail.com
The choice of the optimal muscle relaxant in one-day surgery in children with “small” surgical interventions remains relevant to this day. In modern pediatric surgery, the requirements for the quality of muscle relaxation are highest. However, along with the effectiveness of the drug, its duration and controllability of the action, as well as the safety of use, are important [1-7].
The aim of the study: To determine the pharmacoeconomic rationale for the rational use of muscle relaxants, depending on the duration of operations in one-day surgery in children.
Material and research methods: The study was conducted in surgical clinics of the Azerbaijan Medical University. The study included 156 children who were operated on routinely from 0 to 16 years old (risk of anesthesia I-II ASA), who used combined endotracheal anesthesia during surgery. Based on the requirements of the GCP international program (Good Clinical Practice), the inclusion of children in the study was carried out only after the written consent of the parents. The studied patients were divided into 3 groups depending on the muscle relaxant used: IA (n = 52) - rocuronium bromide (esmeron), IB (n = 52) - atracurium besilate (tracrium), IC (n = 52) - cisatracurius besilate (nimbex). Depending on the type of general anesthesia, these groups were also divided into 2 subgroups: anesthesia based on isoflurane + fentanyl ″ + iso ″ and anesthesia based on sevoflurane + fentanyl ″ + sev ″. The main groups were also divided into 2 age subgroups: children under 2 years of age – IA1, IB1, IC1 and children from 2 to 16 years old – IA2, IB2, IC2.
The distribution of the studied children, depending on the type of general anesthesia, is based on ideas about the potential effect of modern halogen-containing inhalation anesthetics on the duration of action of non-depolarizing muscle relaxants. Moreover, according to the literature, the degree of this influence is different (14-20). So, isoflurane is able to prolong the duration of muscle relaxants by 15% - 20%, and sevoflurane - by 50% - 60% (8-13).
All groups were comparable by age and weight. The duration of anesthesia in various groups is shown in table 1.| Table 1: Distribution of patients according on the duration of surgery and anesthesia. | ||
| Patient groups | Duration of surgery, min | Duration of anesthesia, min |
| IA + sev | 147,5 ± 3,3 | 157,7 ± 5,8 |
| IA + iso | 148,6 ± 3,5 | 168,6 ± 4,5 |
| IB + sev | 150,3 ± 4,4 | 163,3 ± 5,9 |
| IB + iso | 150,1 ± 4,5 | 170,1 ± 6,5 |
| IC+ sev | 149,6 ± 3,6 | 159,6 ± 5,6 |
| IC + iso | 149,2 ± 4,1 | 164,2 ± 5,5 |
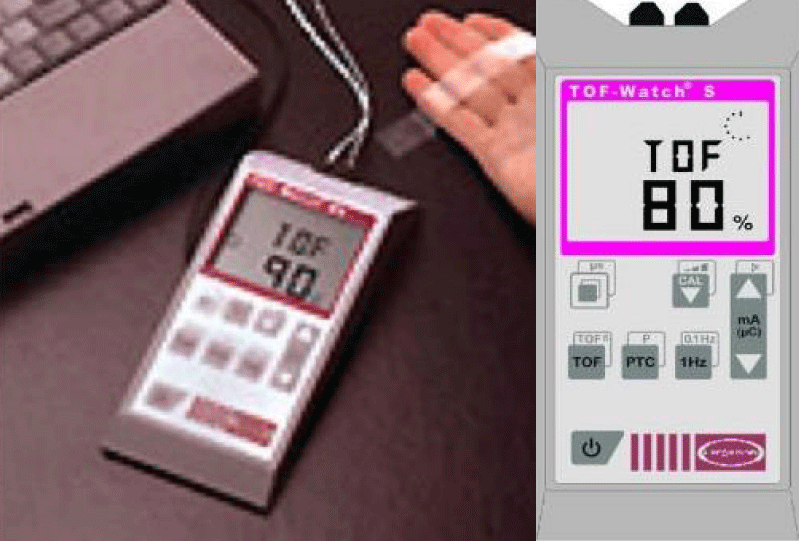
The efficacy and safety of drugs atracurium besilate, cisatracurium besilate, rocuronium bromide was evaluated on the basis of dynamic monitoring of neuromuscular conduction by the accelerometric method (Figure 1).
Figure 1: Neuromonitor TOF-Watch.
To monitor neuromuscular conduction using the TOF-stimulation method, the TOF-watch device was used (Organon Teknika company, producer country, Ireland). The device is equipped with a piezoelectric transducer (accelerometer sensor), which is fixed on the inner surface of the distal phalanx of the thumb of the hand. The state of neuromuscular conduction was evaluated by measuring the electromyographic responses m. adductor pollicis in response to 4 rectangular pulses (each pulse duration - 0.2 ms, interval - 10 sec, frequency of each pulse - 2 Hz) through stimulation electrodes placed on the wrist - proximal (white) and distal (black) (3). We measured the response to the first of 4 stimuli (T1initial) before the introduction of muscle relaxants, the change in the value of T1 with respect to the initial level in percent (T1 / T1initial) and the ratio of the value of the latter to the first response in percent (T4 / T1 or TOF). At an amplitude of 25% of the initial value, the response to the 4th pulse (T4) in TOF disappears. Responses to the 3rd and 2nd impulses (T3 and T2) cease to be recorded at values of T1 = 20% and T1 = 10% of the amplitude, respectively. A clinically stable level of relaxation corresponds to at least 90% decrease in amplitude compared to the initial level (T1≤10%). In this case, only one response to stimulation in TOF mode is detected and satisfactory conditions of muscle relaxation are provided for mechanical ventilation and for the comfortable operation of surgeons. The block depth was calculated as the difference T1initial, taken as 100%, and T1 / T1initial values at a given time. At the stage of restoration of neuromuscular conduction, after the introduction of the last maintenance dose was evaluated (Figure 2).
Figure 2: Monitoring of neuromuscular conduction.
1) the recovery time T1 to 10%, 25%, 75%, 95%, TOF≥75%;
2) the recovery index was calculated – T1 25% -75%.
Clinical recovery criteria were evaluated based on:
1) extubation time – x1;
2) eye opening time – x2;
3) the patient’s readiness for withdrawal from the operating unit – x3;
4) the time from the beginning of extubation until the patient is ready to withdraw from the operating unit – x4 = x3-x1.
It should be noted that intubation and extubation of the trachea was carried out in the presence of appropriate conditions based on clinical symptoms.
Anesthesia technique with modern muscle relaxants
All children included in groups IA, IB, and IC underwent general combined analgesia using inhaled and non-inhaled anesthetics, narcotic analgesics, muscle relaxants, and mechanical ventilation. For the purpose of sedation to all patients in 30 minutes. before the start of anesthesia, midazolam was administered orally at the rate of 0.4 mg / kg, and atropine 0.01 mg / kg intravenously as needed. In children under 3 years of age, the induction of anesthesia was performed with an inhaled anesthetic sevoflurane, and over 3 years old with a non-inhalational anesthetic propofol at a dose of 3.0-3.5 mg / kg. After reaching the state of anesthesia, an intravenous bolus of 0.005% fentanyl was administered at a dose of 3 μg / kg, then after 2-3 minutes, one of the studied muscle relaxants in the main doses. The tracheal intubation process was carried out when a sufficient level of myoplegia was achieved (90% T1 suppression according to TOF-Watch) with the corresponding endotracheal tubes. Tidal volume was calculated from the Radford nomogram. Respiratory rate corresponded to the age norm. All the studied children received a controlled volume of mechanical ventilation (IPPV mode - ventilation parameters that support PetCO2 = 35-40 mm Hg during open operations and PetCO2 = 33-35 mm Hg during laparoscopic operations). Depending on the type and duration of surgery after intubation, a probe was inserted into the stomach and the bladder was catheterized in all children. Maintenance of anesthesia in all patients was carried out under mechanical ventilation on a half-closed circuit with a gas flow from 3.0 to 6.0 l / min depending on age. In the subgroups ″ + iso ″ and ″ + sev ″, one of the inhaled anesthetics 1.0 MAC isoflurane and 1.3 MAC sevoflurane, respectively, was included in the gas mixture. Anesthesia was maintained by fractional administration of 0.005% fentanyl (dose equal to 3-5 μg / kg / h). During the operation, a constant level of myoplegia was achieved due to bolus intravenous injections of a maintenance dose of one of the studied muscle relaxants at T1 up to ≥10%. After surgery, in al l patients in three groups, tracheal extubation was performed during restoration of spontaneous respiration, consciousness, and neuromuscular conduction monitor data (T1≥75% recovery, TOF≥70%). Intraoperative infusion therapy was carried out with crystalloid solutions in volumes corresponding to the age and nature of surgical interventions. As a result of titration of the doses of muscle relaxants studied by us, primary and maintenance doses of muscle relaxants were determined depending on the type of anesthesia (Table 2).
| Table 2: Primary and maintenance doses of muscle relaxants depending on the type of anesthesia | |||
| Type of general anesthesia | Rocuronium bromide, mg / kg | Atracuria besilate, mg / kg | Cisatracuria besilate, mg / kg |
| ″+iso″ | 0,45/0,1 | 0,4/0,15 | 0,12/0,02 |
| ″+sev″ | 0,3/0,1 | 0,3/0,1 | 0,1/0,02 |
Anesthesia with the use of the drug isoflurane (subgroup ′′ + iso ′′)
Given the strong irritating effect of isoflurane on the upper respiratory tract, induction anesthesia in the subgroup ″ + iso ″ was carried out by intravenous administration of propofol at a rate of 3.0-3.5 mg / kg. Upon reaching the surface level of the surgical stage of narcotic sleep, anesthesia is maintained by isoflurane (exposure for 10 minutes). At the stage of tracheal intubation, after intravenous administration of 0.005% fentanyl 3 μg / kg, either rocuronium bromide at a dose of 0.45 mg / kg or atracurium besilate - 0.4 mg / kg or cisatracurium besilate - 0.12 mg / kg was administered. Maintenance of anesthesia in all patients from the subgroup ″ + iso ″ was carried out by 1MAC isoflurane. The maintenance doses of muscle relaxants in children of this group were 0.1 mg / kg in rocuronium bromide, 0.15 mg / kg in atracuria besilate, and 0.02 mg / kg in cisatracuria besilate. Isoflurane was discontinued when skin sutures were applied.
Anesthesia with the use of the drug “Sevoflurane” (subgroup ′′ + sev ′′)
In the ″ + sev ″ subgroups, induction anesthesia was carried out only by inhalation in a half-closed circuit with a gas flow of 2-6 l / min, depending on the age of the child. In all cases, stepwise induction was used, starting from 0.6% to a maximum of 8 vol%. The exposure time was 2-5 minutes; upon reaching complete fall asleep, the content of sevoflurane in the inhaled mixture gradually decreased to the required level of 1.3 MAC on exhalation. After intravenous administration of 0.005% fentanyl at a dose of 2 μg / kg, rocuronium bromide was administered at a dose of 0.3 mg / kg, or atracurium besilate 0.3 mg / kg, or cisatracurium besilate 0.1 mg / kg. Upon reaching 90% suppression of T1, tracheal intubation was performed. Maintenance of anesthesia in all patients of this subgroup was carried out by 1.3 MAC by sevoflurane. Supporting doses of muscle relaxants in children of this group were: rocuronium bromide - 0.1 mg / kg atracurium besilate - 0.1 mg / kg, cisatracuria besilate - 0.02 mg / kg. The supply of sevoflurane, as with isoflurane anesthesia, was stopped at the end of the operation.
Investigation of the effects of rocuronium bromide, atracuria besilate and cisatracuria besilate in the subgroup ′′ + iso ′′
Isoflurane is one of the most widely used inhaled anesthetics at the stage of maintaining general anesthesia in children. The ability of isoflurane to have a sufficiently pronounced and reversible muscle relaxant effect was used by us to develop methods of general anesthesia using low doses of muscle relaxants. We carried out a comparative assessment of the neuromuscular block with titrated doses of rocuronium bromide, atracuria besilate and cisatracuria besilate in combination with 1.3 MAC isoflurane (subgroup ″ + iso ″) at the stages of tracheal intubation, maintenance of general anesthesia and spontaneous restoration of neuromuscular conduction.
Induction in general anesthesia in children of this group was carried out by intravenous administration of propofol until the surgical stage was reached. After switching to the scheme of anesthesia with isoflurane 1.3 MAA and subsequent intravenous administration of 0.005% fentanyl at a dose of 3 μg / kg and the main doses of rocuronium bromide 0.45 mg / kg (1.5x ED95), atracuria besilate 0.4 mg / kg or cisatrcuria Besilate - 0.12 mg / kg (2.5x ED95).
Analyzing the research data, we can say that in young children, the maximum rate of neuromuscular blockade development differed in the rocuronium bromide group at a dose of 0.45 mg / kg. Already after the first minute from the moment of administration, the average values of T1 amounted to 38.9 ± 0.6% of the initial level, with average TOF values of 39.1 ± 1.1%.
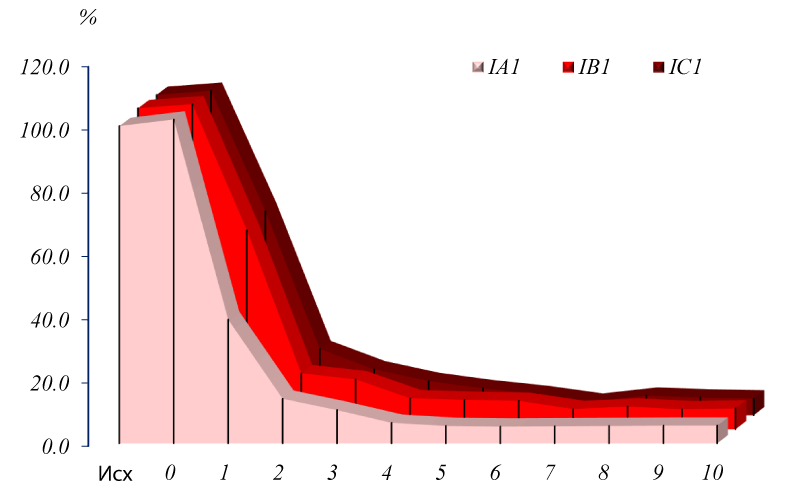
Due to the development of neuromuscular blockade, a decrease in muscle contraction by stimulation progressively increased in patients of this subgroup (Figure 3).
Figure 3: Dynamics of TOF change.
During the first 10 minutes after the introduction of loading doses of muscle relaxants in children under 2 years old in the subgroup ″ + iso ″.
So, by the beginning of the 2nd minute, the maximum suppression of T1 was 4.4 ± 0.6% of the initial data, with average TOF values of 14.1 ± 1.1%. In the subgroup with cisatracuria (IC) at a dose of 0.12 mg / kg, the lowest rate of depression of neuromuscular conduction was observed, where after 1 minute from the moment of administration, T1 was still quite high and averaged 62.5 ± 0.6% from the initial level, with average TOF values of 64.5 ± 24.5%. The introduction of the main dose of 0.4 mg / kg atracuria besilate in the IB subgroup ensured T1 suppression in most patients by the end of the first minute - 56.1 ± 0.6% of the initial level, with average TOF - 63.0 ± 0.6%, which is less than that of rocuronium bromide and cisatracuria besilate.
Further reliable development of neuromuscular blockade also most progressively increased in the subgroup with rocuronium bromide (IA), where already at the 2nd minute in most children 90% T1 suppression was observed on average 4.4 ± 0.6% of the initial level, with average values TOF - 14.1 ± 1.1%. By the second minute in the subgroup with atracuria (IB), the degree of suppression of the first muscle response T1 also approached 90% and averaged 5.3% ± 1.0%, with average TOF values of 17.7 ± 1.1%. In the subgroup of up to 2 years old in children with cisatracuria (IC1), the average values of T1 and TOF were noted at levels of 7.4 ± 1.1% and 17.7 ± 1.1%, respectively, which also indicates a high effectiveness of the drug and the development of neuromuscular blockade in the first 2 minutes from the time of administration of the drug.
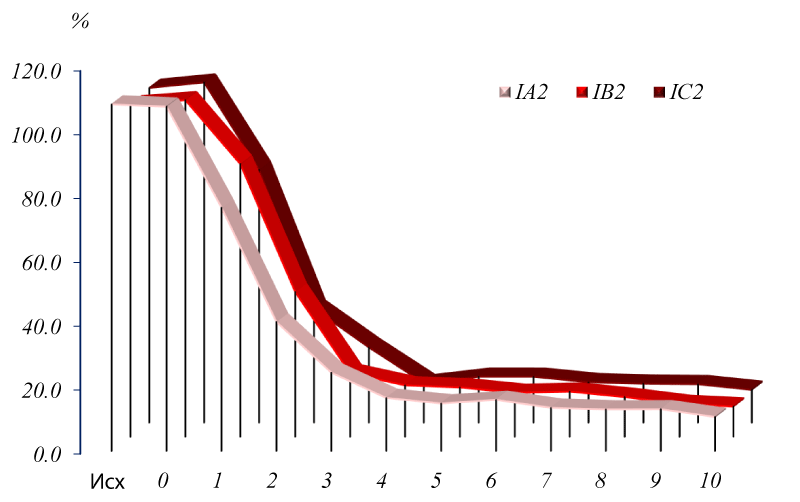
The development of neuromuscular blockade with 90% suppression of T1 in children of the older age group with the highest rate occurred in the group with rocuronium bromide (IA2), so the average values by the second minute –19.6 ± 1.0%, TOF –35.7 ± 1,6%, by the beginning of the 3rd minute from the moment of administration, they were –5.4 ± 0.1% with average TOF values –19.9 ± 0.8%. The dynamics of the development of the neuromuscular block at this stage in children of the older age group IB2 and IC2 were slightly different. So, by the 2nd minute in IB2 with atracurium besilate, the average values of T1 and TOF were –22.9 ± 1.1% and 40.4 ± 1.3%, respectively. The beginning of the 3rd minute from the moment of administration, according to TOF-Watch, was characterized by the rapid development of 90% of neuromuscular blockade in IB2 and IC2 with average values of T1 and TOF: in the subgroup IB2 –7.9 ± 0.3% and 23.6 ± 1,1%, and in the subgroup IC2 - 8.4 ± 0.3% and 24.5 ± 0.9%, respectively (Figure 2).
Consequently, the necessary neuromuscular blockade in many surgical interventions in a large percentage of children created atracuria to besilate by the middle of the second minute, and cisatracuria to besilate only to the end of the second minute. The results of the study showed that, regardless of the type of muscle relaxant used, the maximum T1 suppression in children under 2 years of age is achieved faster than in children over two years of age (Figure 4).
Figure 4: Dynamics of TOF change.
The depth of the neuromuscular block was determined as the difference T1initial taken as 100%, and the ratio T1 / T1initial at a given time. It was determined that the decrease in the main doses of the studied muscle relaxants did not have a significant effect on the depth of development of neuromuscular blockade in children. The greatest depth of the neuromuscular block was also more pronounced in children under 2 years of age than in children of the older age group: in the IA1 subgroup 1.5 ± 0.3% and in the IA2 - 2.5 ± 1.2%, in IB1 - 0, 8 ± 0.7% and IB2 - 1.7 ± 0.9%, IC1 subgroup - 0.7 ± 0.1% and IC2 - 1.8 ± 0.8%, respectively.
Thus, cisatracuria besilate provided the greatest depth of neuromuscular blockade, then atracurium besilate and rocuronium bromide. Therefore, in operations where surgeons require greater muscle relaxation, for example, during laparoscopic interventions, cesatracuria besilate should be preferred from the muscle relaxants studied, since it has a higher blocking effect.
Determination of the duration of a deep neuromuscular block after using the initial dosage of muscle relaxants (recovery period T1 to 10%).
As a result of the analysis of the obtained data, certain differences were revealed depending on age when recording the duration of a deep neuromuscular block (time up to 10% recovery of T1).
Thus, in children under 2 years of age in all subgroups (IA1, IB1 IC1) this indicator was higher, however, a statistically significant difference was obtained only by comparing age subgroups with rocuronium bromide and cisatracuria besilate (p < 0.001). The maximum duration of deep HMB was observed in children aged 2 to 5 months - from 31 to 58 minutes. In children from 6 to 12 months, this time was shorter and ranged from 27 to 51 minutes. As a result, the average time in all children of the subgroup with rocuronium bromide (IA1) was 47.3 ± 5.6 minutes. The smallest duration of neuromuscular blockade in children under 2 years old was observed when using atracuria besilat (IB1), which provided a deep degree of relaxation, on average 35.4 ± 6.4 minutes. In children of the IC1 subgroup, the average time of neuromuscular blockade was 45.6 ± 12.2 minutes.
Variability in the duration of the initial doses of atracuria, cisatracuria besilate and rocuronium bromide was observed in patients in the older age subgroup. So, in children from 3 to 5 years, the duration of deep neuromuscular blockade is slightly higher than in children older than 5 years: in subgroup IB2 - 36.4 ± 8.2 minutes. and 32.2 ± 7.6 min., in the subgroup IC2 - 39.0 ± 6.9 min. and 35.6 ± 8.4 minutes, and in the subgroup IA2 - 21.4 ± 9.8 minutes. and 19.8 ± 10.8 min. respectively. However, a statistical analysis of the results obtained in the older age group did not reveal significant differences (p > 0.05). As a result, the average duration of deep neuromuscular blockade after administration of the initial dose in subgroup IB2 was 33.5 ± 6.6 minutes, in subgroup IC2 - 40.2 ± 7.6 minutes, and in subgroup IA2 - 21.1 ± 1,7 minutes.
After completion of surgical intervention and complete restoration of adequate spontaneous breathing, tracheal extubation was performed for all studied patients. The criteria for the adequacy of spontaneous respiration were indicators of gas exchange and ventilation. After the last maintenance dose of muscle relaxants was administered, the time of T1 recovery to the levels of 25%, 75%, 95% and TOF to 70% and more was estimated. According to the neuromuscular monitoring used by us, the restoration of T1 to the level of 25% took place in all children in all the studied groups.
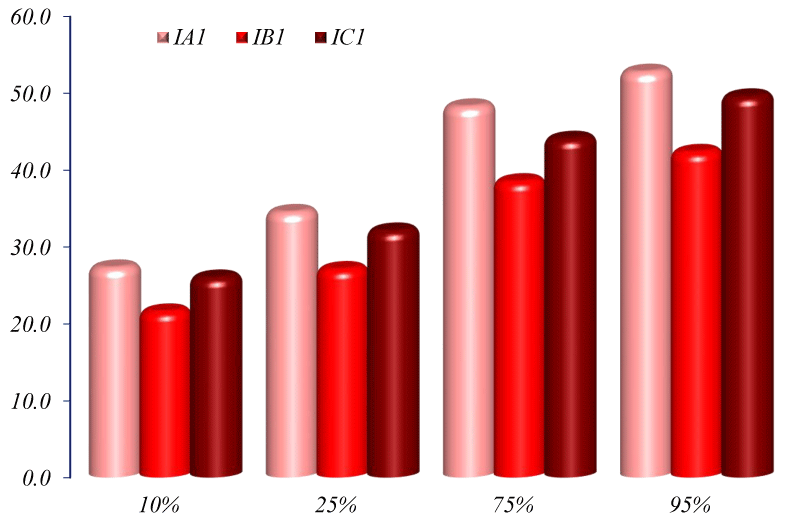
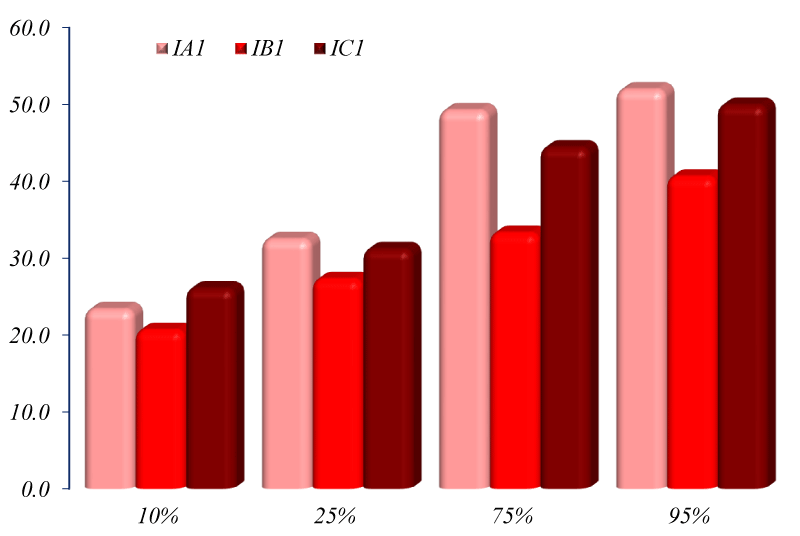
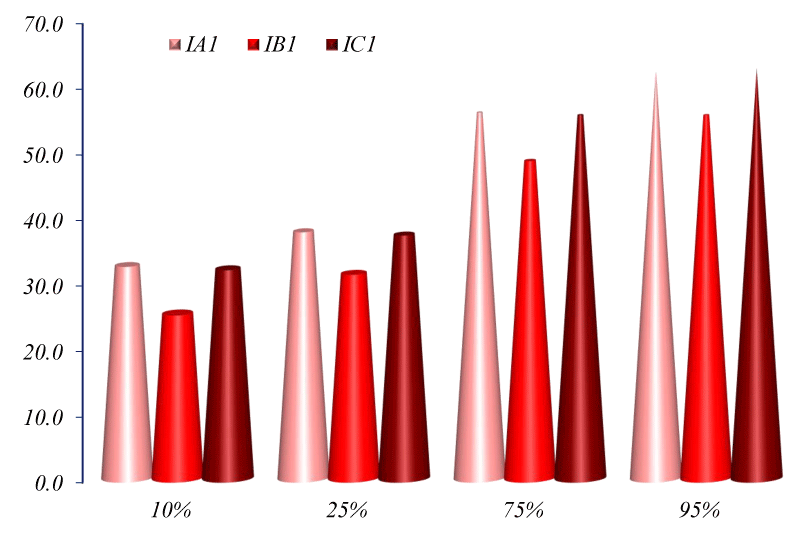
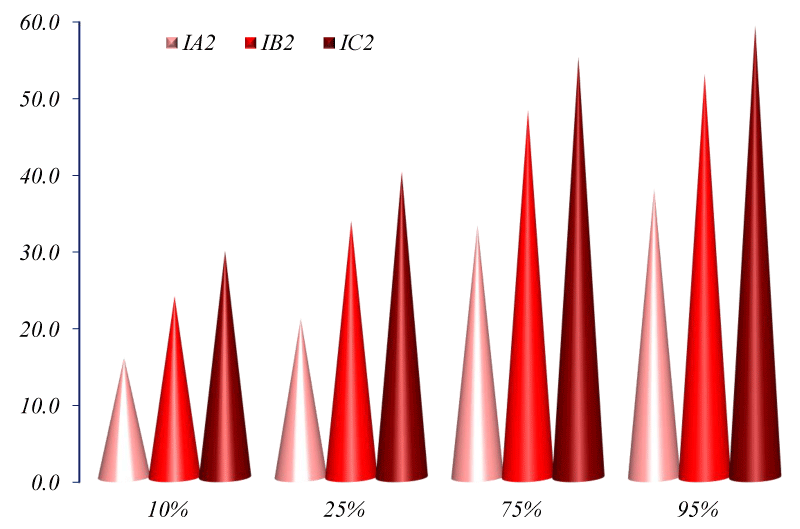
Recovery of T1 to the level of 75% and TOF≥70% in the younger age group occurred only in 21 children (83.1%) in subgroups IA1 and IB1, and in 19 children (75.4%) in subgroup IC1 (Figure 5) In the older age group, T1 recovery to the level of 75% a.nd TOF≥70% was observed in 24 children (93.1%) both in subgroup IB2 and in subgroup IC2. In subgroup IA2, the same degree of recovery occurred in 22 children (Figure 6). Recovery of T1 to the level of 95% was achieved in 21 children (83%) in the subgroup IB1, also in 21 children (83%) in the subgroup IA1, in 22 children (85.5%) in the subgroup IC1. In older age subgroups, this indicator was achieved in 20 children (79.2%) in the subgroup IB2, in 21 children (81.8%) in the subgroup IC2, and in 22 children (84.3%) in the subgroup IA2 (Figures 5,6).
Figure 5: Dynamics of spontaneous recovery of neuromuscular transmission in children under 2 years of age with ″ + iso ″.
Figure 6: Dynamics of spontaneous recovery of neuromuscular transmission in children older than 2 years with ″ + iso ″.
In these children, monitoring was stopped due to the appearance of a negative reaction to hardware electrical stimulation, and extubation was carried out on the basis of clinical signs of restoration of neuromuscular conduction and adequate spontaneous ventilation.
And in this subgroup, the restoration of neuromuscular conduction after the last dose of muscle relaxants was administered in all cases was spontaneous and did not require the use of anticholinesterase drugs. In no case was prolongation of the neuromuscular block observed.
An analysis of the results showed that the highest, on average, the rate of spontaneous recovery of neuromuscular conduction in children under 2 years old was noted in subgroup IB1 (atracuria besilata), and the lowest in subgroup IA1 (rocuronium bromide). Recovery time after the administration of the last maintenance dose of cisatracuria besilate is in the middle position and approaches the results of rocuronium bromide. The smallest fluctuations in the results were observed in the younger age subgroup IA1 (rocuronium bromide), where in children under 5 months the time of spontaneous recovery was longer than in children from 6 months to 3 years. In the younger age subgroups IB1 (atracuria) and IC1 (cisatracuria), the variation in results was significantly less. Significant differences in time were obtained at all stages of recovery (except for T1 25% -75%) only when comparing the younger age subgroups IA1 (rocuronium bromide) and IB1 (atracurium): atracurium
Comparative evaluation of the dynamics of the development of neuromuscular blockade with sevoflurane
Sevoflurane is the most used inhalation anesthetic in pediatric anesthesiology. The ability to quickly and comfortably induce, a very high level of safety and a high elimination rate are the main criteria for choosing sevoflurane in multimodal combined anesthesia in children. In addition to the direct effect on contractility of the striated muscle, sevoflurane significantly enhances and prolongs the neuromuscular effects of non-depolarizing muscle relaxants, which can significantly reduce their dosage.
The dynamics of the development of BMD within 10 minutes after intravenous administration of the main doses of the studied muscle relaxants are shown in table 3.
| Table 3: The dynamics of changes in T1 and TOF during the first 10 minutes after administration of loading doses of muscle relaxants in children under 2 years old in the subgroup ″ + sev ″. | ||||
| Time, min | Indicators | IA1 (rocuronium bromide) | IB1 (atracurium besilat) | IC1 (cisatracurium besilat) |
| Initial data | Т1 | 102,0 ± 0,5 | 102,5 ± 0,4 | 101,6 ± 0,5 |
| ТОF | 103,4 ± 0,5 | 103,5 ± 0,5 | 100,5 ± 0,5 | |
| 0 | Т1 | 100,6 ± 0,4 | 101,2 ± 0,5 | 100,5 ± 0,5 |
| ТОF | 101,4 ± 0,4 | 103,6 ± 0,4 | 103,7 ± 0,4 | |
| 1 | Т1 | 58,2 ± 0,6 * | 64,8 ± 0,6 * | 67,3 ± 0,6 * |
| ТОF | 59,3 ± 1,1 * | 67,3 ± 0,5 * | 74,1 ± 0,5 * | |
| 2 | Т1 | 8,6 ± 0,6 * | 12,3 ± 0,6 * | 12,6 ± 0,5 * |
| ТОF | 17,1 ± 1,1 * | 25,4 ± 1,1 * | 27,8 ± 0,9 * | |
| 3 | Т1 | 5,8 ± 0,5 * | 8,7 ± 0,5 * | 8,8 ± 0,8 * |
| ТОF | 9,1 ± 0,6 * | 12,5 ± 0,6 * | 16,2 ± 0,7 * | |
| 4 | Т1 | 5,4 ± 0,3 * | 5,7 ± 0,6 * | 5,8 ± 0,6 * |
| ТОF | 7,6 ± 0,5 * | 10,5 ± 0,5 * | 11,5 ± 1,1 * | |
| 5 | Т1 | 3,1 ± 0,4 * | 6,6 ± 0,5 * | 5,3 ± 0,5 * |
| ТОF | 4,3 ± 0,5 * | 9,2 ± 0,5 * | 10,1 ± 1,1 * | |
| 6 | Т1 | 2,3 ± 0,3 * | 3,1 ± 0,4 * | 4,1 ± 0,5 * |
| ТОF | 4,8 ± 0,6 * | 8,1 ± 0,5 * | 8,6 ± 0,7 * | |
| 7 | Т1 | 2,2 ± 0,3 * | 3,7 ± 0,3 * | 3,9 ± 0,4 * |
| ТОF | 6,1 ± 1,1 * | 7,5 ± 1,1 * | 8,3 ± 1,1 * | |
| 8 | Т1 | 2,3 ± 0,4 * | 2,7 ± 0,5 * | 3,1 ± 0,6 * |
| ТОF | 4,5 ± 0,6 * | 7,8 ± 0,6 * | 7,5 ± 0,6 * | |
| 9 | Т1 | 2,8 ± 0,4 * | 2,5 ± 0,5 * | 3,5 ± 1,0 * |
| ТОF | 4,4 ± 0,6 * | 7,4 ± 0,6 * | 8,1 ± 2,5 * | |
| 10 | Т1 | 2,2 ± 0,5 * | 2,5 ± 0,6 * | 2,6 ± 0,6 * |
| ТОF | 6,5 ± 1,1* | 8,3 ± 0,5* | 8,1 ± 0,8* | |
| Note: statistical significance of differences in indicators with respect to the initial data: * - p < 0.001. | ||||
Analyzing the data of the first 2 minutes from the moment of administration, we can see that the average T1 suppression rate in children under two years of age turned out to be comparable in all the studied muscle relaxant groups. However, some advantage of rocuronium bromide has been identified. By the end of the 1st minute from the moment of administration of rocuronium bromide at a dose of 0.3 mg / kg, according to TOF-Watch, the average T1 in the IA1 subgroup was 58.2 ± 0.6%, with average TOF - 59.3 ± 1.1%.
The degree of suppression of T1 in other younger age subgroups at this point in time was slightly different: in the subgroup IB1 - 64.8 ± 0.6%, with average TOF – 67.3 ± 0.5%, in the subgroup IC1 – 67.3 ± 0.6%, with an average TOF of –74.1 ± 0.5%. Further, the development of neuromuscular blockade progressively increased, and by the end of the 2nd and beginning of the 3rd minute from the moment of the introduction of relaxants, T1 suppression of 90% took place in all children of the younger age group. At the same time, rocuronium bromide was superior to others in the rate of achieving maximum blockade of neuromuscular conduction. So, the average values of T1 in the subgroup IA1 were 8.6 ± 0.6%, with average TOF values of 17.1 ± 1.1%. In the subgroups IB1 and IC1, the same indicators were: 12.3 ± 0.6% with average TOF –25.4 ± 1.1% and 12.6 ± 0.5% with TOF –27.8 ± 0.9 %, respectively (Figures 7,8).
Figure 7: Dynamics of TOF changes during the first 10 minutes after the administration of loading doses of muscle relaxants in children under 2 years old in the subgroup ″ + sev ″.
Figure 8: Dynamics of changes in TOF during the first 10 minutes after the administration of loading doses of muscle relaxants in children over 2 years old in the subgroup ″ + sev ″
As a result, the average time from the moment of completion of the initial dose of muscle relaxant administration to the moment of the maximum neuromuscular blockade (T1 suppression of 95% - 100%) in children under two years old was: in the IA1 subgroup (rocuronium bromide) - 1.8 ± 0.3 min ., in the subgroup IB1 (atratcurium) - 2.0 ± 0.4 minutes, and in the subgroup IC1 - 2.6 ± 0.6 minutes. The maximum suppression of T1 in all subgroups was comparable and amounted to, on average, 9.7 ± 2.5% in the range from 97% to 99%.
As can be seen from the data presented in older age subgroups, the rate of development of maximum neuromuscular blockade was lower than in children under 2 years of age, and to achieve T1 suppression of 95% - 100% it took more time.
By the end of the 2nd minute from the moment of administration of muscle relaxants, the following were noted: in the IB2 subgroup - 27.3 ± 0.4% with TOF indices - 44.1 ± 1.1%; in the IC2 subgroup - 37.5 ± 0.5%, with TOF indices - 49.8 ± 1.1%; in subgroup IA2 - 18.6 ± 0.5%, with TOF values - 32.9 ± 1.1%. In the period of the 3rd minute from the moment of administration only in the subgroup with rocuronium bromide, the majority of children developed the maximum neuromuscular blockade, where the average values of T1 were 5.6 ± 0.6% with average TOF values of 16.5 ± 0.6%. In the atracuria and cisatracuria besilate subgroups, the maximum neuromuscular blockade in most children developed only in the 4th minute, where T1 indices were: in the IB2 subgroup - 4.5 ± 0.5%, with average TOF - 14.8 ± 0, 6%; in the subgroup IC2 - 6.6 ± 0.5%, with average TOF –18.1 ± 0.6%.
As a result, the highest average rate of achieving maximum T1 suppression was noted in the rocuronium bromide subgroup (IA2) - 2.4 ± 0.5 min., Compared with the atracuria besilate (IB2) subgroups - 3.0 ± 1.3 min. and cisatracuria besilate (IC2) - 3.5 ± 0.8 min. Moreover, an analysis of the results of the study showed that in all older age subgroups, the minimum time to reach the complete neuromuscular block, according to TOF-Watch, was observed in children aged 2 to 5 years (range from 1.8 minutes to 4.6 minutes). And the maximum is for children over 8 years old (range from 2.3 minutes to 5.3 minutes).
The maximum suppression of T1 in all older age subgroups was also comparable and amounted to an average of 96 ± 2.7%, with a range from 95% to 100%.
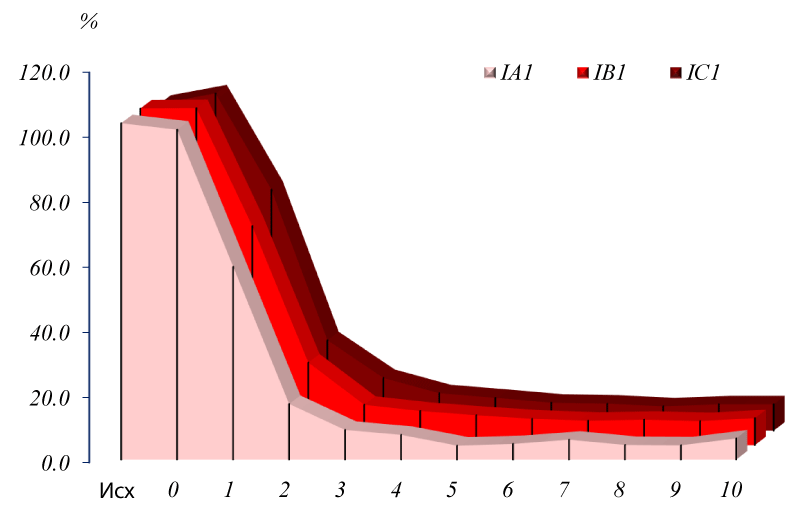
The recovery period of neuromuscular conduction in the group with ″ + sev ″
Extubation of the trachea after completion of surgery and restoration of adequate spontaneous breathing was performed in all children. According to the results of neuromuscular monitoring, restoration of T1 to 25% took place in all children in all the studied subgroups. Recovery of T1 to 75% and TOF>70% - in children under 2 years of age, only 20 children (76.8%) in subgroups IB1 and IA1 took place, and in 19 children (72.3%) in subgroup IC1. In the older age group, T1 recovery to 75% and TOF>70% was observed only in 23 children (91.1%), both in subgroup IB2 and in subgroup IC2. In subgroup IA2, the same degree of recovery occurred in 22 children (86.7%).
The data presented indicate that in children under 2 years of age, spontaneous restoration of neuromuscular conduction after the use of atracuria, cisatracuria besilate and rocuronium bromide is subject to a certain effect of sevoflurane, and to a different extent. In particular, the recovery index (T1 25-75%) after the administration of the last maintenance dose in atarkuria and cisatracuria besilate increased by 33.5% and 33.6%, respectively, and in rocuronium only by 23.7% when compared with the subgroups ″ + iso ″, this confirms that inhaled anesthetics to a greater extent prolong the effects of benzylisoquinoline muscle relaxants (atracuria and cisatracuria besilate). The total time of complete recovery (T1 0% - 95%) in the atracuria besilate subgroup (IB1) was the shortest and averaged 55.4 ± 1.8 minutes. The same time was longer in the subgroups of cisatracuria and rocuronium bromide and amounted to 62.5 ± 1.2 minutes and 61.8 ± 1.6 minutes, respectively.
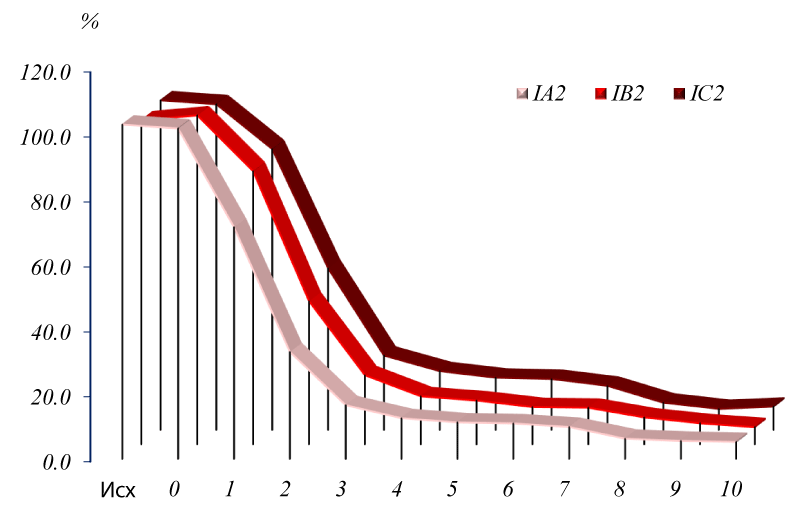
However, statistical analysis did not reveal significant differences between relaxants - p > 0.05 (Figure 9).
Figure 9: Dynamics of spontaneous recovery of neuromuscular conduction in children under 2 years of age with ″ + sev ″.
The result of the study showed an increase in the recovery index in this subgroup by 23.8% relative to the performance of the subgroup ″ + iso ″. In addition, in the atracuria subgroup (IB2), the average duration of complete spontaneous recovery was 52.6 ± 1.8 min versus 58.9 ± 1.8 min in the cisatracuria subgroup (IC2), which was statistically significant (p < 0.05). The recovery index in these subgroups relative to the subgroup ″ + iso ″ also increased by 22.5% in atracurium besilat and by 28.7% in cisatracurium besilat (Figure 10).
Figure 10: Dynamics of spontaneous recovery of neuromuscular conduction in children older than 2 years with ″ + sev ″.
Under conditions of general anesthesia with the inclusion of 1.3 MAC of isoflurane, reduced basic doses of non-depolarizing muscle relaxants provide deep neuromuscular blockade for 30-40 minutes.
Based on the results obtained, it can be concluded that a single administration of 0.3 mg / kg rocuronium bromide, 0.3 mg / kg atracurium and 0.1 mg / kg cisatracurium besilate when combined with sevoflurane provide quality conditions for performing smooth tracheal intubation and Mechanical ventilation in children of all age groups.
The duration of the clinically effective action of the studied muscle relaxants in the indicated doses in children under 2 years of age allows for quality relaxation during operations performed both traditionally and laparoscopically for a duration of 30-50 minutes. To ensure a comfortable working environment for surgeons during laparoscopic operations in children over 2 years old, the main doses of muscle relaxants should be at least 0.4 mg / kg for atracurium, 0.12 mg / kg for cisatracurium and 0.45 mg / kg for rocuronium bromide.
The combination of sevoflurane and low doses of the studied muscle relaxants avoids the prolonged restoration of neuromuscular conduction and awakening, which as a result saves working time and speeds up the operating room during small surgeries in children under one-day surgery.
- Ali MZ, Ebied RS, Atallah MA, El Sabea HHA, El Monaemb AA, et al. Cisatracurium dose-response relationship in patients with chronic liver disease. Egy J Anaesthe. 2014; 30: 197-202.
- Alonso A, De Boer H, Booij L. Reversal of rocuronium-induced neuromuscular block by sugammadex in neonates. Eur J Anaesthesiol. 2014; 31: 163
- Bhananker SM, Treggiari MM, Sellers BA, Cain KC, Ramaiah R, et al. Comparison of train-of-four count by anesthesia providers versus TOF-Watch SX: a prospective cohort study. Can J Anesth. 2015; 62: 1089-1096. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26224034
- El-Kasaby M, Atef H, Helmy A, Abo El-Nas M. Cisatracurium in different doses versus atracurium during general anesthesia for abdominal surgery. Saudi J Anaesth. 2010; 4: 152-157. PubMed: https://pubmed.ncbi.nlm.nih.gov/21189851
- Kendrick J, Carr R, Ensom M. Pharmacokinetics and drug dosing in obese children. J Pediatr Pharmacol Ther. 2010; 15: 94-109. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3018176/
- Meretoja O. Neuromuscular block and current treatment strategies for its reversal in children. Paediatr Anaesth. 2010; 20: 591-604. PubMed: https://pubmed.ncbi.nlm.nih.gov/20642658
- Mohamed N, Cynthia A. Lien: pharmacology of muscle relaxants and their antagonists chapter 29 / Ronald D. Miller’s Anaesthesia. Churchill Livingston. 2010: 868-890.
- Movafeghetal A. Cost analysis and safety comparison of Cisatracurium and Atracurium in patientsundergoing general anesthesia. European Review for Medical and Pharmacological Sciences. 2013; 17: 447-450. PubMed: https://pubmed.ncbi.nlm.nih.gov/23467941
- Naguib M. Neuromuscular blocking drugs and reversal agents / In: Flood P, Rathmell J, Shafer S. eds. Stoelting’s Pharmacology & Physiology in Anesthestic Practice. 5th ed. Philadelphia, PA: Wolters Kluwer Health. 2015: 323-344.
- Plaud B, Meretoja O, Hofmockel R, Raft J, Stoddart PA, et al. Reversal of rocuronium-induced neuromuscular blockade with sugammadex in pediatric and adult surgical patients. Anesthesiology. 2009; 110: 284-294. PubMed: https://pubmed.ncbi.nlm.nih.gov/19194156
- Shang G, Wang N, Qing Q, Jun G. Clinical pharmacology of cisatracurium during nitrous oxide-propofol anesthesia in children. J Clin Anesthe. 2008; 20: 411-414.
- Thilen S, Bhananker S. Qualitative neuromuscular monitoring: how to optimize the use of a peripheral nerve stimulator to reduce the risk of residual neuromuscular blockade. Curr Anesthesiol Rep. 2016; 6: 164-169. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4963456/
- Todd M, Hindman B. The implementation of quantitative electromyographic neuromuscular monitoring in an academic anesthesia department: Follow-up observations. Anesth Analg. 2015; 121: 836-838. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26287308
- Zuche H, Morinello E, Viestenz A, Fiorentzis M, Seitz B et al. Reduction of intraocular pressure and ocular pulse amplitude during general anesthesia. Ophthalmology. 2015; 112: 764–769. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25510627
- M. J. Murray, H. DeBlock, B. Erstad, Gray AW Jr, Jacobi J, et al. Clinical practice guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med. 2016; 44: 2079–2103. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28069681
- Moss M, Huang DT, Brower RG, Ferguson ND, Ginde AA, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. New Engl J Med. 2019; 380: 1997–2008. PubMed: https://pubmed.ncbi.nlm.nih.gov/31112383/
- Bouju P, Tadie JM, Barbarot N, Letheulle J, Uhel F, et al. Clinical assessment and train-of-four measurements in critically ill patients treated with recommended doses of cisatracurium or atracurium for neuromuscular blockade: a prospective descriptive study. Ann Intensive Care. 2017; 7: 10. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5247382/
- Warr J, Thiboutot Z, Rose L, Mehta S, Burry JD, et al. Current therapeutic uses, pharmacology, and clinical considerations of neuromuscular blocking agents for critically ill adults. Ann Pharmacother. 2011; 45: 1116-1126. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21828347
- Lundstrøm LH, Duez CH, Nørskov AK, Rosenstock CV, Thomsen JL, et al. Avoidance versus use of neuromuscular blocking agents for improving conditions during tracheal intubation or direct laryngoscopy in adults and adolescents. The Cochrane database of systematic reviews. 2017. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28513831
- Palsen S, Wu A, Beutler SS, Gimlich R, Yang HK, et al. Investigation of intraoperative dosing patterns of neuromuscular blocking agents. J Clin Monitoring Computing. 2018. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30094585