Research Article
Quantification of the pressures generated during insertion of an epidural needle in labouring women of varying body mass indices

Wee MYK1*, Isaacs RA2, Vaughan N3, Dubey VN4 and Parker B5
1Consultant Anaesthetist, Department of Anaesthesia, Poole Hospital, NHS Foundation Trust, Longfleet Road, Poole BH15 2JB, United Kingdom
2Consultant Anaesthetist, Department of Anaesthesia, Southampton University Hospital, Tremona Road, Southampton, SO16 6YD, United Kingdom
3Post-doctorate Researcher, Bournemouth University, Faculty of Science and Technology, Poole House, Talbot Campus, Fern Barrow, Poole BH12 5BB, United Kingdom
4Professor of Robotics, Bournemouth University, Faculty of Science and Technology, Poole House, Talbot Campus, Fern Barrow, Poole BH12 5BB, United Kingdom
5Consultant Anaesthetist, Department of Anaesthesia, West Hertfordshire NHS Trust, Watford General Hospital, Vicarage Road, Watford, Hertfordshire WD18 0HB, United Kingdom
*Address for Correspondence: Wee MYK, Professor, Department of Anaesthesia, Poole Hospital, NHS Foundation Trust, Longfleet Road, Poole BH15 2JB, United Kingdom, Tel: +44 1202 442443; Email: m.wee@virgin.net
Dates: Submitted: 20 November 2017; Approved: 30 November 2017; Published: 01 December 2017
How to cite this article: Wee MYK, Isaacs RA, Vaughan N, Dubey VN, Parker B. Quantification of the pressures generated during insertion of an epidural needle in labouring women of varying body mass indices. Int J Clin Anesth Res. 2017; 1: 024-027. DOI: 10.29328/journal.ijcar.1001004
Copyright License: © 2017 Wee MYK, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Epidural; Pressures; Simulation; Obstetrics
Abstract
Objective: The primary aim of this study was to measure pressure generated on a Tuohy needle during the epidural procedure in labouring women of varying body mass indices (BMI) with a view of utilising the data for the future development of a high fidelity epidural simulator. High-fidelity epidural simulators have a role in improving training and safety but current simulators lack a realistic experience and can be improved.
Methods: This study was approved by the National Research Ethics Service Committee South Central, Portsmouth (REC reference 11/SC/0196). After informed consent epidural needle insertion pressure was measured using a Portex 16-gauge Tuohy needle, loss-of-resistance syringe, a three-way tap, pressure transducer and a custom-designed wireless transmitter. This was performed in four groups of labouring women, stratified according to BMI kg/m2: 18-24.9; 25-34.9; 35-44.9 and >=45. One-way ANOVA was used to compare difference in needle insertion pressure between the BMI groups. A paired t-test was performed between BMI group 18-24.9 and the three other BMI groups. Ultrasound images of the lumbar spine were undertaken prior to the epidural procedure and lumbar magnetic resonance imaging (MRI) was performed within 72h post-delivery. These images will be used in the development of a high fidelity epidural simulator.
Results: The mean epidural needle insertion pressure of labouring women with BMI 18-24.9 was 461mmHg; BMI 25-34.9 was 430mmHg; BMI 35-44.9 was 415mmHg and BMI >=45 was 376mmHg, (p=0.52).
Conclusion: Although statistically insignificant, the study did show a decreasing trend of epidural insertion pressure with increasing body mass indices.
Introduction
High-fidelity epidural simulators have a potential role in improving training. The “Curriculum for a CCT in Anaesthetics” stated that “the historical reliance upon workplace-based learning is being compromised further by decreasing hours spent in the clinical setting. This and other factors combine to encourage the use of simulation to enhance learning” [1]. Simulation is gaining popularity not only for creating mock scenarios but also in learning psychomotor skills [2-5].
Existing simulators have shown some utility but there is still potential for further improvement if the positive attributes of each could be drawn together to create a high fidelity simulator. This was the conclusion reached by our team in a review article on epidural simulators where user feedback from existing simulators highlighted the unrealistic sensation of needle advancement, particularly at the point of loss-of-resistance [6]. The primary aim of this study was to quantify pressures generated during epidural needle insertion in parturients of varying BMI in a bid to incorporate these measured epidural insertion pressures into a simulator. This measurement will address the deficiency of unrealistic sensation of needle advancement in a proposed high fidelity epidural simulator. Ultrasonography and MRI of the parturients’ lumbar spine will enable the acquisition of detailed anatomical imaging linked to the measured epidural insertion pressures which may aid training of epiduralists during simulation by creating a visual three-dimensional display of relevant structures on a computer screen with realistic feel of epidural insertion.
The importance of how we teach neuraxial analgesia and anaesthesia stems from the fact that epidural analgesia can result in significant patient morbidity. The epidural procedure has been shown to require a high degree of skill and dexterity. The incidence of permanent harm (vertebral abscess, haematoma and nerve injury) from obstetric epidurals ranged from 0.2 to 1.24 in 100,000 [7]. Two large studies of obstetric epidural complications reported that, although rare, life-threatening complications do occur [8,9]. Post-dural puncture headache (PDPH) has a more frequent occurrence of approximately 1% with other studies quoting a higher incidence of 2.8% [10,11]. Changes to training and compliance with European Working Time Directive create fewer opportunities for anaesthetists to learn technical skills. Recent reviews comment on the poorly structured system for teaching skill acquisition and highlight the shift away from practising on patients due to reduced tolerance for error [12-14].
The current obesity epidemic poses greater challenges with significantly more attempts needed to site epidurals by anaesthetists with reduced experience. Analgesic failure and epidural re-sites are more likely [15-18]. The ability to practice simulation of patients with various body mass indices may assist in the learning process and reduce the learning curve. A survey of anaesthetic trainee members of the Obstetric Anaesthetists’ Association in 2013 conducted by our team revealed that learning the epidural technique generates marked stress and anxiety and trainees strongly support training on epidural simulators [19]. By developing a novel epidural simulator to provide realistic needle insertion feedback coupled with detailed anatomical imaging, we hope to improve the training in epidural technique, reduce the learning curve and also reduce patient morbidity.
Methods
This study was approved by the National Research Ethics Service Committee South Central, Portsmouth (REC reference 11/SC/0196). Participants were women admitted to Poole Maternity Hospital delivery suite. Women who had expressed an interest in epidural analgesia at an early stage during their labour were recruited after obtaining written informed consent. Parturients were divided into four sub-groups according to their BMI, which was calculated from their current weight and height. (kg/m2). The four sub-groups were as follows; BMI 18-24.9; BMI 25-34.9; BMI 35-44.9 and BMI >=45. A sample size of 20 parturients was selected for this observational study, with five in each BMI sub-group to represent the measurements of the sub-groups. The recruits were not randomised and measurements were undertaken when the two experienced anaesthetic researchers were available.
Healthy nulliparous or multiparous labouring women, more than 18 years of age with singleton pregnancies were included. Exclusion criteria included absolute contraindication to epidural analgesia, known spinal abnormalities, previous back surgery, history of connective tissue disorders, women who needed their epidural re-siting or where there were doubts regarding communication or understanding of the study.
Following study consent and prior to the epidural procedure, an ultrasound scan of the lumbar spine was performed using the Sonosite® M-Turbo™ ultrasound machine by the trained researcher. The images were recorded and stored for later use in the development of a proposed high fidelity simulator. When epidural analgesia was requested, as is standard practice, verbal informed consent was obtained after the parturient was provided with information from the Poole Maternity epidural information card. The parturient was placed in the sitting position and the epidural procedure was conducted using strict aseptic technique by one of two experienced anaesthetists who have performed in excess of 250 successful lumbar epidurals (R.I. and B.P.). The epidural space was located using a Portex 16-gauge Tuohy needle (Smiths Medical, Kent, UK) at either the L2/L3 or L3/L4 interspaces using the midline approach. These are clinically the commonest spinal levels for epidural anaesthesia. Pressure was applied to the plunger of the saline-filled loss of resistance syringe as the needle traversed the lumbar interspace until the epidural space was located using the ‘loss of resistance’ (LOR) technique whereby the plunger pressure rapidly reduces upon entering the epidural space. The exact technique adopted by the two epiduralists was not specified and they used a mixture of constant pressure and intermittent pressure techniques. Measurement of the epidural pressures was recorded in between contractions (detected from the continuous tocograph tracing) via a sterile three-way tap (BD ConnectaTM) connected between the saline-filled loss of resistance syringe and Tuohy needle with a metre long saline-filled pressure manometer tubing linked to a pressure transducer (Kimal, London, UK). Recording of the epidural needle insertion pressures was undertaken wirelessly using an in-house system described and tested in our pilot porcine trial [20]. This ensured that the privacy of the parturient as only the research epiduralist and midwife were present in the room. Insertion pressure measurements ceased after epidural space identification. An epidural catheter was inserted and epidural analgesia was commenced as per Poole Maternity Unit guidelines.
An MRI scan of the lumbar spine was performed within 72 hours of delivery at the convenience of the parturient. Images were stored for further analysis at the end of the trial. All MRI lumbar scans were performed using a sequence known as VISTA (Philips Healthcare, Surrey, UK) which is a three-dimensional, T2-weighted, turbo spin echo with isotropic spatial resolution sequence. An experienced MRI radiographer and radiologist identified the ligamentum flavum (LF) from the images with a member of the research team using software on the Philips Ingenia 3.0T MRI scanner (Philips Healthcare, Surrey, UK). Images were taken in the longitudinal plane and reconstructed into a transverse view. After localization of the LF, a region of interest (ROI) within the ligament was drawn at the presumed level of epidural insertion. This enabled calculation of the minimum, maximum and mean image intensity for each selected ROI and a histogram of intensity distribution plotted for each parturient.
Analysis of Variance (ANOVA) was applied to compare the maximum pressure between the four BMI groups. This was unbalanced one-factor analysis as it involved the factor BMI and the effect of BMI on insertion pressure. Since the study had 4 BMI groups, analysis involved four levels of the BMI factor. One-way ANOVA was applied because the sample contained more than 2 BMI group levels. The design was targeted to meet principles of replication and randomisation. The aim of ANOVA was to estimate the amount of variation due to assignable causes (variance between BMI groups) as well as due to chance causes (variance within BMI groups). Paired t-test was used to compare the mean insertion pressures between the 4 BMI groups.
Results
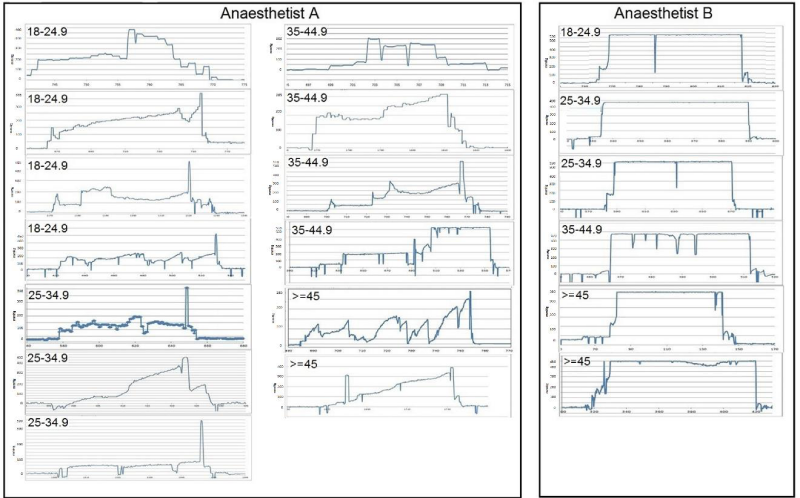
Epidural insertion pressure traces were recorded in 19 out of 20 labouring women (Figure 1). We could not complete a full set of measurements and imaging within the BMI >=45 sub-group as the study period ended before we could recruit the last participant. For each parturient, the peak (maximum) pressure was measured at the point just before LOR and the lowest (minimum) pressure was recorded when the reading stabilised after initial insertion. It was interesting to note that Anaesthetist A used a combined intermittent and constant pressure epidural technique whereas anaesthetist B used predominantly constant pressure technique to identify the epidural space.
During recording of the epidural insertion pressures, certain events within the graph such as interspinous ligament entry and piercing the ligamentum flavum may occur in a different place with respect to time for each patient. Due to this, the activity timing cannot be controlled in the same way for each participant. Further, the data cannot be combined time-wise so only the minimum and maximum pressure values are compared.
When each parturient was recruited, regardless of their BMI stratification, they were assigned to whichever operator was on duty and therefore not randomised. The mean values for each group in Table 1 include a mixture of epidural insertion pressures measured from either anaesthetist A or B. The number of parturients assigned to each anaesthetist (A and B) also varied between groups and anaesthetist A performed the majority of the epidurals due to availability. An interesting finding was the differences in the actual epidural technique arising from the resultant display of the epidural pressure traces between the two experienced anaesthetists, one using predominantly an intermittent technique (anaesthetist A) whilst the other a constant pressure technique (anaesthetist B); Figure 1.
Figure 1: Epidural needle insertion pressure traces of the two epiduralists on labouring women of varying BMI showing two different techniques of epidural insertion.
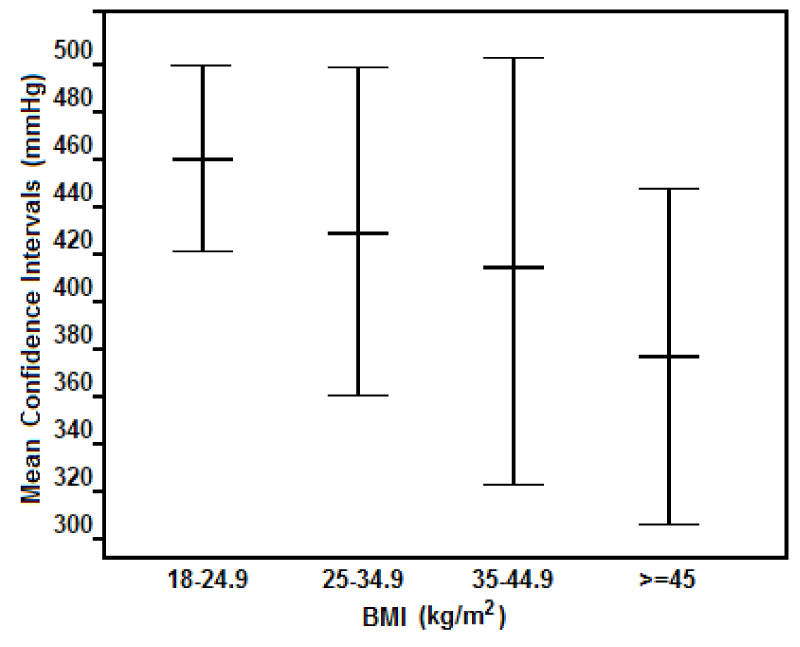
The minimum, maximum and mean value for each group was tabulated in Table 1. For each parturient, the peak pressure measurement was visible at the point just before LOR. The results suggest a trend towards lower mean pressures as the BMI gradually increases. The confidence intervals in Figure 2 show the range for each BMI group inside of which we can be 95% confident that the population mean falls.
| Table 1: The needle insertion pressures (mmHg) and BMI group. | ||||
| BMI sub-group (kg/m2) |
Max Pressure (mmHg) | Mean Max Pressure (mmHg) and (Standard Deviation) | Min Pressure (mmHg) |
Mean Min Pressure (mmHg) and (Standard Deviation) |
| 18-24.9 | 480 385 460 450 530 |
461 (46) | 200 125 90 100 150 |
133 (39) |
| 25-34.9 | 390 430 320 490 520 |
430 (79) | 100 80 60 0 0 |
48 (41) |
| 35-44.9 | 300 285 510 510 470 |
415 (101 | 50 0 50 50 0 |
30 (24) |
| >=45 | 280 400 380 450 |
376 (71) | 50 0 50 0 |
25 (25) |
One-way ANOVA was used to compare difference in needle insertion pressure between the BMI groups. The resulting p-value of 0.52 suggests that there were no statistically significant differences between BMI groups. A paired t-test was performed between BMI group 18-24.9 and the three other BMI groups. The observed difference between the sample means in the pressure measurement dataset was not significant (p>0.10).
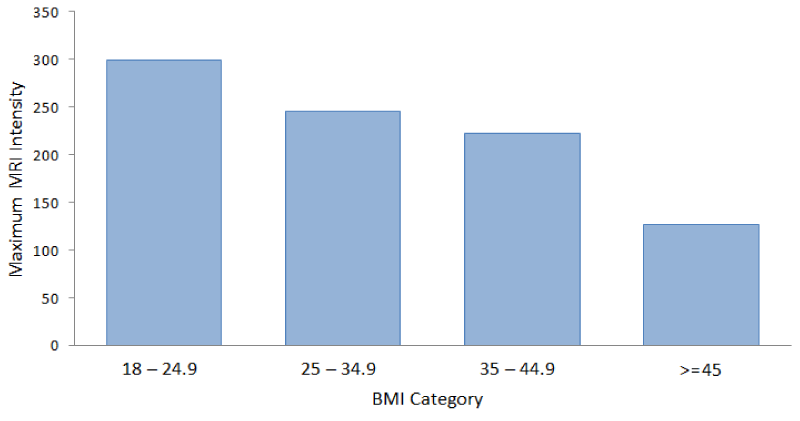
The study also used T2-weighted MRI data to differentiate on the basis of intensity in which fat, water and fluid are brightest. This allows the intensity to be used to identify the content of tissue. The size of the region of interest (ROI) varied from patient to patient, ranging from 11-43 pixels, which equates to an area of tissue size 9–37 mm2. The tissue in the ROI was selected within the visible part of the ligamentum flavum, which is responsible for the highest insertion pressure before reaching the epidural space. The MRI intensity represents the strength of the MR signal. The stronger the MR signal, the brighter the region within the image. There has been recent evidence that MRI data can enable tissue density quantification [21]. Tissue density may affect the pressures measured during insertion of Tuohy needle.
To check the variation further, ANOVA was conducted upon the analysis of the MRI intensity between BMI groups. MRI scans were undertaken in 17 of the 19 study participants as one parturient refused to have an MRI, despite earlier consenting to the imaging procedure and one parturient with a BMI>=45 had a novel gastric band device in-situ and we were uncertain of its compatibility with MRI. The paired t-test was performed for MRI ligamentum flavum intensity comparing BMI group 18-24.9 to the other groups. There was no significant difference in MRI ligamentum flavum intensities between BMI groups (p=0.4). As BMI increases, maximum MRI intensity of the ligamentum flavum is seen to decrease based on analysis of ROI at the presumed insertion level of the epidural needle (Figure 3). However, statistical analysis has shown that this is not significantly different between groups.
Discussion
This clinical study measured a range of epidural needle insertion pressures in labouring parturients of varying BMI. Although statistical analysis revealed no significant trend between BMI groups, the measured data will be useful for incorporating into high fidelity epidural simulators to replicate a realistic in vivo experience. Tran and colleagues used a complicated pressure measuring system to record the forces applied during epidural insertions in 11 parturients with BMI ranging from 25 to 30 using a 17-gauge Tuohy needle with glass syringe for LOR [22]. Due to differences in method, technique and equipment we could not accurately compare the results of their study with ours, although reference to previously reported pressures when the needle tip is in the ligamentum flavum for adults does confirm similarity with our data [21].
In an attempt to elucidate the density of the ligamentum flavum in parturients with varying BMI, we analysed MRI scans of the ligamentum flavum in the four groups. By utilising image intensity in the selected ROI and through the creation of intensity histograms, we were able to infer details of ligament composition and density. The interpretation of this limited data has to be taken with caution. The statistical analysis showed no significant change in MRI intensity of the ligamentum flavum with increasing BMI.
Anaesthetist A conducted the majority of the pressure measurements and was also involved in the initial porcine study but had two inadvertent dural punctures during the course of the study using a combined intermittent and constant pressure technique. Anaesthetist B, who joined the study at a later stage, used a pure constant pressure technique and did not have any dural taps in the six study epidural pressure measurements. This finding may be coincidental but it opens a discussion of the possible merits of the constant pressure technique versus intermittent technique in terms of potential risk of inadvertent dural puncture. The signature pressure traces in a simulator scenario could potentially be utilized for training techniques and honing skills and should be the subject of further study.
A complete description of forces involved during needle insertion is complex. In particular, there is interplay between the reaction forces from the needle shaft in tissue versus reaction forces from the plunger of the syringe. Both are critical for a simulator to reproduce in order to have as close to an in vivo experience as possible. The complex needle insertion forces include tip/cutting forces, shaft friction and non-axial forces and torques. The plunger force includes the needle orifice/tissue interface, syringe friction, syringe leakage and saline compression. It is extremely challenging to accurately quantify these minute forces but we believe that the measured resultant insertion pressure represented a good surrogate [19]. A secondary aim of this study was to utilise the pressure data, ultrasound and MRI images for incorporation into a novel high fidelity epidural simulator. This would increase the realistic feel of the simulated epidural procedure, whilst assessing the skill of the epiduralist by measuring not only their success rate in reaching the epidural space without breaching the dura but also the details of the technique utilized. We have reviewed all the past and present commercially available epidural simulators and concluded that none have the required high-fidelity characteristics to enhance training in the epidural procedure [6]. From the data acquired specifically related to pressure measurement, we would be able to integrate this important variable into the proposed model. Further work will involve developing and evaluation of this proposed high-fidelity epidural simulator and the analysis of epidural pressure traces related to technique and risk of morbidity.
In conclusion, we have been able to quantify the pressures generated during insertion of a Tuohy needle in labouring women of varying BMI. Differing epidural insertion pressures between parturients of varying BMI may be related to differences in ligamental and tissue structures.
Funding
The Obstetric Anaesthetists’ Association (OAA) via the National Institute for Academic Anaaesthesia (NIAA) supported this work with a grant (Application ID WKR0-2012-0035).
Author’s Contribution
M.Y.K.W and R.A.I: Study design, ethics approval, recruitment and epidural pressure measurements and analysis of the data; N.V. and V.D. design of the remote pressure measurement receiver and transmitter, recording and statistical analysis of the data; B.P. recruitment and epidural pressure measurements. M.Y.K.W. wrote the original manuscript and all authors contributed to the amendments and agreed the final version.
Acknowledgements
We would like to thank Helen Reid, senior MRI radiographer, Poole Hospital NHS Foundation Trust and Dr. Angus Wood, Consultant Radiologist for their input into the analysis of the MRI scans. We would like to thank Prof. Peter Thomas, Professor of Healthcare Statistics and Epidemiology, Bournemouth University, for his statistical advice.
Trial registry number: ISRCTN 01054711 and REC reference 11/SC/0196; 13 June 2011.
*Presented in part at the Obstetric Anaesthetists’ Association Annual Meeting, Dublin, Ireland, May 2014
References
- Royal College of Anaesthetists. Curriculum for a CCT in Anaesthetics, version 2. London. 2010. Ref.: https://goo.gl/RjbRCi
- Bruce RCH, McLeod ADM, Smith GB. A survey of UK anaesthetic trainee attitudes towards simulator based training experience. Bulletin of the Royal College of Anaesthetists. 2005; 34: 1722-1723. Ref.: https://goo.gl/RM27DZ
- Gaba DM. Improving Anesthesiologists’ Performance by Simulating Reality. Anesthesiology. 1992; 76: 491-494.
- Zausig YA, Bayer Y, Hacke N, Sinner B, Zink W et al. Simulation as an additional tool for investigating the performance of standard operating procedures in anaesthesia. Bri J Anaesth. 2007; 99: 673-678. Ref.: https://goo.gl/HNUWNT
- Kneebone RL, Nestel D, Vincent C, Darzi A. Complexity, risk and simulation in learning procedural skills. Medical Education. 2007; 41: 808-814. Ref.: https://goo.gl/GhxQXw
- Vaughan N, Dubey VN, Wee MYK, Isaacs RA. A review of epidural simulators: where are we today? Med Eng Phys. 2013; 35: 1235-50. Ref.: https://goo.gl/UMiJ1R
- Cook TM, Counsell D, Wildsmith JAW. Major complications of central neuraxial block: report on the Third National Audit of The Royal College of Anaesthetists. Bri J Anaesth. 2009; 102: 179-190. Ref.: https://goo.gl/XjAPnp
- Paech MJ, Godkin R, Webster S. Complications of obstetric analgesia and anaesthesia: a prospective analysis of 10,995 cases. Int J Obstet Anesth. 1998; 7: 5-11. Ref.: https://goo.gl/aJTwam
- Jenkins JG. Some immediate serious complications of obstetric analgesia and anaesthesia: a prospective study of 145,550 epidurals. Int J Obstet Anesth. 2005; 14: 37-42. Ref.: https://goo.gl/obXK7s
- Gleeson CM, Reynolds F. Accidental dural puncture rates in the UK. Int J Obstet Anesth. 1998; 7: 242-246. Ref.: https://goo.gl/JHMRNV
- Gupta S, Collis R, Harries S. Increasing dural tap rate: is this a national trend? International Journal of Obstetric Anesthesia. 2007; 16: 17.
- Grantcharov TP, Reznick RK. Teaching procedural skills. BMJ. 2008; 336: 1129-1131. Ref.: https://goo.gl/sDxP7E
- Smith TS, Johannsson HE, Sadler C. Trials of labour: can simulation make a difference to obstetric anaesthetic training? Current Anaesthesia and Critical Care. 2005; 16: 289-296. Ref.: https://goo.gl/57KpYd
- Aggarwal R, Darzi A. Technical skills training in the 21st century. New Eng J Med. 2006; 355: 2695-2696. Ref.: https://goo.gl/HWxFq1
- Bamgbade OA, Khalaf WM, Ajal O, Sharma R, Chidambaram V et al. Obstetric anaesthesia outcome in obese and non-obese parturients undergoing caesarean delivery: an observational study. Int J Obstet Anesth. 2009; 18: 221-225. Ref.: https://goo.gl/3U36u4
- Perlow JH, Morgan MA. Massive maternal obesity and perioperative caesarean morbidity. Am J Obstet Gynecol. 1994; 170: 560-565. Ref.: https://goo.gl/2KYVGP
- Hood DD, Dewan DM. Anesthetic and obstetric outcome in morbidly obese parturients. Anesthesiology. 1993; 79: 1210-1218. Ref.: https://goo.gl/EvgPTt
- Dresner M, Brocklesby J, Bamber J. Audit of the influence of body mass index on the performance of epidural analgesia in labour and the subsequent mode of delivery. BJOG. 2006; 113: 1178-1181. Ref.: https://goo.gl/dLZzGB
- Isaacs RA, Wee MYK, Dubey VN, Vaughan N. Current training in epidural analgesia: a survey of UK practice. Poster presented at Obstetric Anaesthesia 2013. Bournemouth. 2013; UK. Ref.: https://goo.gl/rGU5UT
- Vaughan N, Dubey VN, Wee MYK, Isaacs RA. Towards a realistic in vitro experience of epidural Tuohy needle insertion. Proceedings of the Institute of Mechanical Engineers. Part H: J Eng Med. 2013; 227: 767-777. Ref.: https://goo.gl/t43mL2
- Rodeira J, Calabuig R, Aliaga L, Espinosa W, Hobeich F et al. Mathematical analysis of epidural space location. Int J Clin Monitoring Computing. 1995; 12: 213-217. Ref.: https://goo.gl/paciJj
- Tran D, Hor KW, Kamani AA, Lessoway VA, Rohling RN. Instrumentation of the loss-of-resistance technique for epidural needle insertion. IEEE Transactions of Biomedical Engineering. 2009; 56: 820-827. Ref.: https://goo.gl/wUwCwE